The most obvious application of this new technique is in patients who may have suffered a stroke or other brain injury. Stroke is the Number 2 cause of death and the biggest reason for the neurological deficit in adults. If a stroke occurs, it is essential to be able to image the part rapidly and with high fidelity in any patient. Since the outcome worsens with each minute of delay, the ability to image the brain and initiate treatment at the first point of contact with the patient would affect both survival and the ultimate prognosis for functional survival very significantly. The same applies to almost any form of brain injury.
.jpg)
Earlier techniques
Magnetic resonance imaging (MRI) is the technique of choice for getting high-resolution images of the brain. It can help evaluate a host of brain disorders, including stroke, brain cancer, and traumatic brain injury.
The problem with MRI, accurate as it generally is, is that it cannot be used if the patient has a metallic implant or a foreign body. It is also impossible with patients who are severely claustrophobic, very obese, or uncooperative for any reason. X-ray computed tomography (CT) is the next best option but exposes the patient to ionizing radiation. Both these modalities require large equipment, which is expensive, cannot be brought to a sick patient's bedside, and are therefore difficult to use in patients presenting with emergency conditions that involve altered consciousness, such as suspected stroke.
Co-researcher Parashkev Nachev says, "The practicalities of MRI will always limit its applicability, especially in the acute setting, where timely intervention has the greatest impact. Neurology has been waiting for a new, universally applicable imaging modality for decades: full-waveform inversion could well be the answer."
If the current device can be proven to produce accurate images in clinical trials, the emergency imaging and diagnosis of such patients will become very much more straightforward. Moreover, the new imaging tool can help monitor very sick patients continuously.
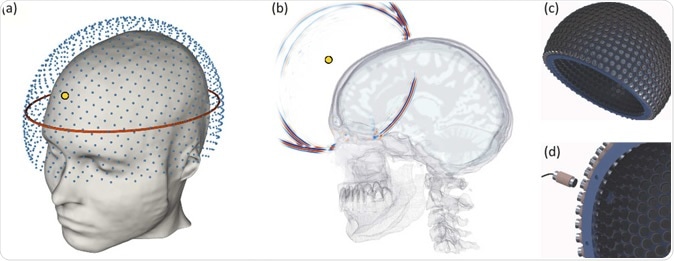
How the prototype helmet could image the brain. Image Credit: Imperial College London
Seismic imaging in brain disorders
Earth scientists use seismic data as well as full waveform inversion techniques (FWI), which provide a picture of the Earth's interior. This is by supplying seismic data from earthquake detectors or seismometers to FWI algorithms that, in turn, represent 3D images of the Earth's crust, which can be used to predict earthquakes and to detect oil or gas reservoirs deep within the crust.
The new study harnesses this capability to carry out medical imaging by using sound waves to generate a high-resolution image of the brain. The tool depends on sound waves, the technology already used in ultrasound scanning. However, ultrasound cannot penetrate bone as well as the refractive aberrations caused by the contrast between the skull and the brain. The new imaging device can overcome this barrier.
This is now available, thanks to the new technology. According to study author Lluis Guasch, "An imaging technique that has already revolutionized one field - seismic imaging - now has the potential to revolutionize another - brain imaging."
Other experts chip in, like Bryan Williams, who directs the NIHR UCL Hospitals Biomedical Research Center, "This is an extraordinary development which has huge potential to provide accessible brain imaging to evaluate the brain in head trauma, stroke and a variety of brain diseases. It is also a fabulous illustration of how the collaboration between engineers and clinicians, using methods from another sphere of science, can bring ground-breaking innovation into medical care."
The acoustic imaging helmet
The device is a helmet lined with rows of sound transducers that generate ultrasonic energy that is transmitted through the head of the patient. The energy propagated is recorded and fed into a computer through the helmet. The data is then processed using FWI algorithms to create a three-dimensional image of the skull's interior.
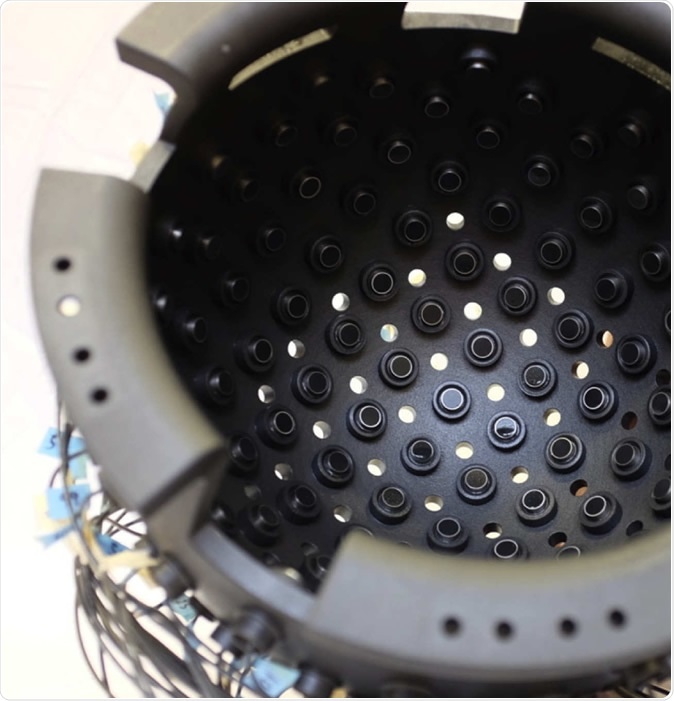
The prototype helmet. Image Credit: Imperial College London
The prototype was tested on a human without any known brain pathology. The results showed that it produced a high-quality recorded signal that could be used to display a full image of the part examined. The investigators say they feel sure that the scattered energy from the brain can be interpreted in a clinically useful way.
Moreover, the use of computer modeling helps them to achieve high-quality imaging at low sound frequencies that will be safe to the brain yet capable of penetrating the skull. With the help of such modeling techniques, they have generated computer simulations showing the details of various brain tissues, to prove that sound waves can create a high-resolution image of the brain.
The device is smaller, faster, cheaper, and easier than those used in most other imaging techniques, which means it can be used for portable imaging as in ambulances. The use of FWI can prevent distortion due to noise while allowing the use of low frequencies.
Implications
Commenting on the device, Guasch says, "This is the first time FWI has been applied to the task of imaging inside a human skull. FWI is normally used in geophysics to map the structure of the Earth, but our collaborative, multidisciplinary team of earth scientists, bioengineers, and neurologists are using it to create a safe, cheap and portable method of generating 3D ultrasound images of the human brain."
Nachev goes on to explain, "This is a vivid illustration of the remarkable power of advanced computation in medicine. Combining algorithmic innovation with supercomputing could enable us to retrieve high-resolution images of the brain from safe, relatively simple, well-established physics: the transmission of soundwaves through human tissue." To establish their thesis, scientists must now build a prototype that will provide live images from the normal human brain. This will be the first stage in the journey to a full-scale testable device to be used on real patients.
The study concludes: "The potential value of FWI imaging is threefold. It could improve outcomes in acute neurological disorders by enabling earlier intervention. Second, the low cost, high safety, portability, and high resolving power of the technology provides the ability to monitor the brains of patients continuously at the bedside. And third, the technology can be deployed readily and safely in a wide range of situations where neuroimaging would be desirable but is currently unavailable—for example, within developing nations with limited health budgets, in remote locations, routinely at contact-sports events, within military deployments, or as part of disaster relief when local infrastructure is compromised."
Journal reference:
Guasch, L., Calderón Agudo, O., Tang, M. et al. Full-waveform inversion imaging of the human brain. npj Digit. Med. 3, 28 (2020). https://doi.org/10.1038/s41746-020-0240-8