The researchers looked at the happenings in and around COVID-19 positive women. They took an epidemiological and clinical profile of each of them, using inpatient records, interviews, and field studies. The aim was to mirror the way the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spreads and how people interact. The scientists also used overseas open-source data for overseas cases.
It was on the last day of the year 2019 that a group of people with viral pneumonia was diagnosed in Wuhan, China. The illness was later termed coronavirus disease 2019 or COVID-19. Later on, cases multiplied in Wuhan, suggesting that community spread had occurred. The outcome was a lockdown of Wuhan and then of other cities in the province.
By January 30, 2020, the World Health Organization (WHO) had declared it a public health emergency of international concern. Over the next month, the spread included almost 100,000 cases and nearly 3,400 deaths.
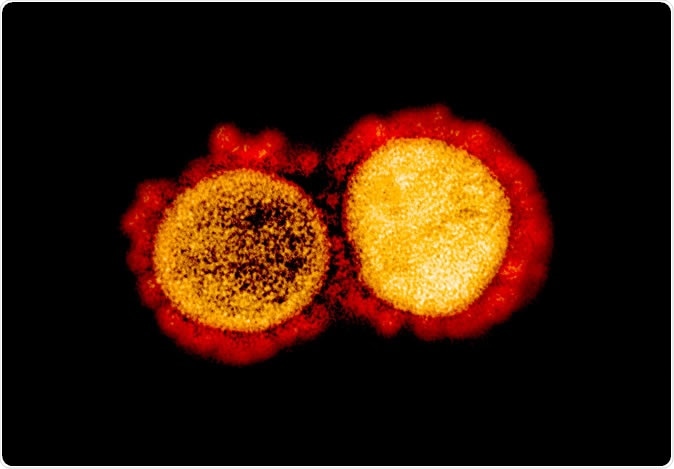
Novel Coronavirus SARS-CoV-2 Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
The Singapore response
Singapore began early on to prepare for the inevitable cases to limit the spread. On January 23, 2020, the government confirmed the first case – the same day flights from Wuhan to Singapore stopped. By February 22, 2020, there were almost 90 Singapore residents with the infection.
The first 18 cases among these were recent travelers to Wuhan. Moreover, the scientists in Singapore traced three contact clusters arising from a Chinese tour group, a conference held by a company, and a church.
The research aimed to answer questions:
- How infectious is the virus?
- How does it spread, and how can we limit its spread?
- How can we enhance surveillance and the detection of new cases?
The study also attempts to find the incubation period of the SARS-CoV-2 and the period over which one case spreads to the next – a transmission pair. The researchers interviewed confirmed cases to find their demographic profile, their symptoms, and the patterns of activity over the 14 days before symptoms appeared until the patient was isolated in a hospital.
The investigators also performed contact tracing, finding people who spent reasonable amounts of time within 2m of a confirmed case (close contacts), and other contacts. The close contacts were quarantined for 14 days from the time of last exposure to the confirmed case, at home or in quarantine facilities with daily monitoring, and isolation with testing if symptoms developed. Home-quarantined individuals were video-called three times daily to verify their location, and if needed, continuous tracking devices were used to tag those who went outside regardless of quarantine. Other contacts were put on phone surveillance or self-monitoring, as required by their level of risk.
They asked the confirmed patients whether they could have had contact with overseas confirmed cases in the two weeks before the first symptoms were observed. They also used open-source data to track secondary spread within each of the clusters of cases.
The findings
The study showed that 36 cases of COVID-19 occurred in relation to the first three clusters of local spread. These were identified by the Ministry of Health in Singapore on February 3, February 5, and February 8, 2020. The researchers traced possible contact routes in all the clusters and were able to find the median incubation time to be four days. The serial interval for the transmission within a single-family was 3-8 days.
They also found that about 31% of transmission pairs were linked to a single person while there was no spread with 32 of the cases.
The most common symptoms were fever and cough in 88% and 82% of patients, respectively. About 70% developed lung opacities on chest X-ray. Lymphopenia and thrombocytopenia occurred in a significant number of people. Most people experienced resolution over a few days, but viral shedding from the nasopharynx continued for 3-9 days. Two patients developed acute respiratory distress and had to be intubated and shifted to the intensive care unit. No deaths were recorded.
Despite the use of thermal screening on flights from Wuhan, and later on, all flights from China, the cases which initiated transmission within these clusters were probably undetected as they entered Singapore as their temperature was normal at the time. These cases were probably from China before the Wuhan lockdown.
Surveillance necessary to block transmission
The scientists say that any country with a high rate of travel to and from China should have a vigorous surveillance program to look for cases not just among those who have been in China but also in their contact community. Such rapid and thorough surveillance followed by immediate quarantine of close contacts will ensure that transmission through that chain ends there.
The fact remains that among 425 close contacts of COVID-19 cases, two only developed the illness, but most did not. The authors say this raises “he hypothesis that a few spreading events can result in clusters of transmission, whereas for most cases, the transmission ended.”
Secondly, the global sharing of data on cases is essential to seek out cases and contain transmission.
Thirdly, there was prolonged interaction between the suspected index case and the contacts who subsequently became ill. Thus, the virus might be directly transmitted via surfaces touched by both the patients and others. Hand hygiene is, therefore, paramount in interrupting the chain of transmission.
The authors conclude, “It is important for countries to do active case-finding among close contacts of cases to prevent clusters from spreading.”
Journal reference:
Pung, R., Chiew, C. J., Young, B. E., et al. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. The Lancet 2020. https://doi.org/10.1016/S0140-6736(20)30528-6