Researchers have been studying the ongoing pandemic of COVID-19 caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) closely since its beginning in December 2019. To date, the virus has infected over 850,000 individuals across the globe and killed over 41,000.
Most experts agree that when infected with the novel coronavirus, 80 percent will have a mild illness. Associate Professor Sanjaya Senanayake, an infectious diseases specialist from the Australian National University, said: "in most individuals, there will be a mild to moderate illness that lasts about two weeks." In some, however, the disease process can be severe.
The World Health Organization (WHO) also agrees that 15 percent of individuals infected with coronavirus can develop severe infections needing oxygen supplementation. Ventilation is needed in 5 percent of the severe infections, says the WHO.
Dr. Senanyake said, "For COVID-19 at the moment, the global case fatality rate is over 3 percent, although we think it's probably closer to 1 percent." However, all experts in this field agree that the final mortality rate or killing capacity of the infection is yet to be determined conclusively.
How does the infection occur?
This virus or the SARS-CoV-2 virus has spike proteins on its surface. These proteins bind to specific receptors in the hosts. After binding, the viral proteins enter the host cells by breaking open the cell membrane. Then, like most infective viruses, it utilizes the host cell machinery to create more viral particles until it breaks open the cell and kills it. The virus acts to inactivate the body's defense system or the immune system leading to widespread inflammation.
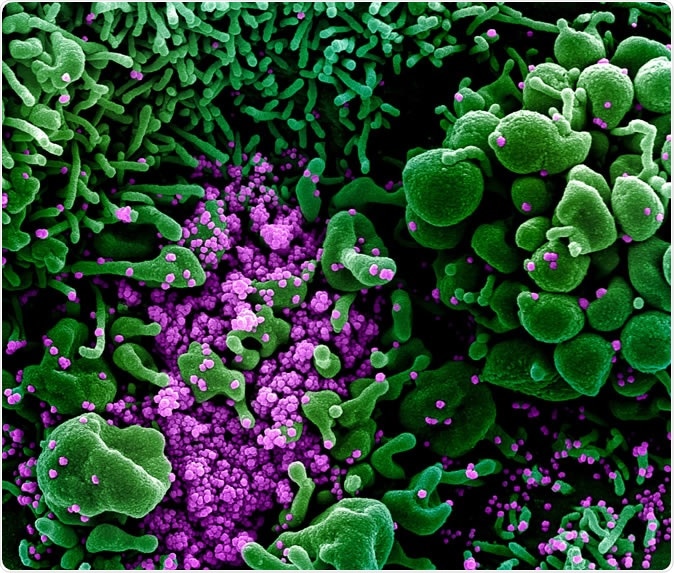
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of an apoptotic cell (green) heavily infected with SARS-COV-2 virus particles (purple), isolated from a patient sample. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
Experts have said that, like in most viral infections, it is this inflammation that manifests as the symptoms such as fever, cough, headache, sore throat, etc. In many infected persons, there may be no symptoms at all. In some, however, the inflammation takes the upper hand, and there is progressive damage to the lungs leading to fatigue and shortness of breath.
Soon the immune system goes into overdrive. Large number of viruses can trigger the over activation of the immune system, and now the inflammation goes beyond control. Cytokines are chemicals secreted within the body. These have been implicated in this over-activity of the immune system. The air sacs in the lungs can fill with fluid, and there is an advancement of viral pneumonia that further leads to shortness of breath and difficulty in breathing.
Virologist Professor William Rawlinson from the University of New South Wales, explained, "If you have something like a boil you get a lot of fluid and if that's happening inside your lung ... then that clearly interrupts exchange of oxygen between the atmosphere and your blood."
The WHO says that SARS can attack the body in three phases:
- Viral replication
- Immune over-activity
- Lung destruction
As a next step, the multiplying viruses within the infected person can break and harm the linings of the lungs, and this opens up a portal for bacteria to enter into the lungs and cause more severe bacterial infections. Oxygen levels in the blood start to drop as the lungs are compromised, and this causes damage to other organs such as the heart. The bacterial infection, along with pneumonia, worsens, and spread to the bloodstream affecting other organs such as the kidneys and leads to severe fall in blood pressure and sepsis. This can cause multiorgan damage and, eventually, failure.
Who are at risk of these severe effects of the virus?
Not everyone develops severe consequences of the COVID-19 infection. Some people, though, are more at risk.
Persons who have been traveling to a country or region where the infection has been typically more severe such as China, Iran, Italy, Spain, the United States, Korea, etc. are at a higher risk of getting the infection. Persons who have been in close contact with persons who have been diagnosed to be positive cases of COVID-19 are also at a higher risk of getting the infection.
The risk of severe disease is more significant among vulnerable populations such as the elderly, those with chronic medical conditions such as heart disease, diabetes, lung diseases such as asthma, chronic obstructive lung disease (COPD), etc. Aboriginal and Torres Strait Islander people have also been found to have higher rates of chronic ailments and are thus at greater risk. Persons with cancer and those with a suppressed immune system are also at a higher risk of getting viral infection and developing severe symptoms.
However, the virus has been known to infect and even kill people who are in their thirties, forties or fifties. Children have been known to be carriers of the infection but are less affected by the infection compared to adults.
Epidemiologist Professor Robert Booy of the National Centre for Immunisation Research and Surveillance (NCIRS) warns that increasing age can be a significant risk factor. He said, "The other thing that loads the risk on top of being old is those chronic conditions like diabetes, heart disease, hypertension. If you have [these conditions], and you're elderly, you're in trouble."
Virologist Professor Rawlinson explained that intensive care and ventilation might be necessary for those with severe disease. Elderly, he explained, may be too weak and frail to be able to sustain the ravages of the infection and the widespread inflammation and often succumb to be. He and others warn that while some of these individuals could be saved, the paucity of intensive care beds for them as there is an overwhelming number of cases can be the reason they die.
The idea is to flatten the infection rate curve and prevent an overburdening of the healthcare system with cases of COVID-19. Washing hands frequently, covering mouth and nose while sneezing or coughing, disinfection of the surfaces in and around the house and workspaces and avoidance of contact with other persons with the infection can help protect from the infection, they add. As of now, vaccine trials are underway, and no specific drugs have been found to be 100 percent effective in treating this infection.