The currently raging COVID-19 pandemic is taking thousands of lives around the globe, mostly due to respiratory failure. While approximately 80% of those who become symptomatic after becoming infected by the causative agent, the SARS-CoV-2 virus, will not need to be hospitalized, the rest will need medical attention and often intensive care because of acute lung injury, or the acute respiratory distress syndrome (ARDS). The only treatment for these patients is supportive care, including mechanical ventilation.
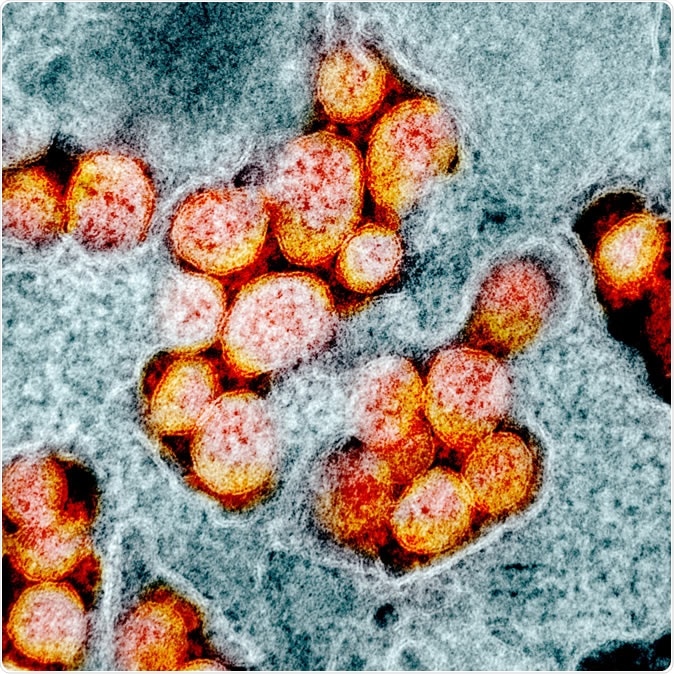
Novel Coronavirus SARS-CoV-2 Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
As the unprecedented pandemic threatens to overwhelm the world's medical facilities, an increasing number of patients are being admitted with complications of the novel coronavirus disease. Public health experts have predicted that as the situation worsens, the number of cases in the United States might go into the thousands, forcing doctors to make difficult decisions on mechanical ventilation.
However, the number of ventilators is far too few for the demand, all around the world, triggering a search for effective therapies when ventilators aren't available or aren't sufficient to provide relief. Against this backdrop, a drug more commonly used to treat strokes and heart attacks caused by blood clots is coming to the forefront. Called tissue plasminogen activator (tPA), the drug is a clot-dissolving agent.

Ventilator equipment for artificial respiration. Image Credit: Andrij Vatsyk / Shutterstock
Why is tPA useful in COVID-19-associated ARDS?
Data flowing in from the analysis of cases in China and Italy indicate the development of marked aberrations in the blood clotting process in people with severe COVID-19 illness. Such patients seem to have microthrombi within the tiny blood vessels supplying the lung alveoli, keeping the capillaries from filling with blood. This prevents proper gas exchange, and the blood oxygen levels drop drastically.
The good thing about tPA is that it is a drug already approved by the Food and Drug Administration (FDA), and is therefore already well studied for safety. Repurposing such a drug is comparatively easy, and such therapies can make it to the mainstream relatively fast.
A small human study in 2001 on patients with terminal respiratory distress reduced the fatality rate from the expected 100% to 70%. Further exploration of the drug in this setting was not carried out, but the current situation warrants such trials.
The study
Anecdotal evidence about abnormal clotting around catheters and IV lines observed in a section of COVID-19 patients with Acute Respiratory Distress Syndrome (ARDS) suggested the use of tPA, a natural anti-coagulant which was approved by the FDA in 1996 for patients with heart attack, stroke, and pulmonary embolism. However, the role of the drug in reducing ARDS-related casualties has been debated in medical research for nearly two decades, leading researchers at the BIDMC to consider its use in COVID-19 ARDS patients experiencing aggressive clotting.
The current study reports the beginning of a clinical trial to assess the role of tPA in the treatment of COVID-19 patients with acute respiratory distress syndrome (ARDS), led by a team of physicians-scientists from Beth Israel Deaconess Medical Center (BIDMC). The research is approved under the FDA's 'compassionate use' approval program, which allows the use of experimental drugs in patients who have no other options for treatment.
The drug will be given intravenously and/or via direct instillation into the airways. A bolus dose over 2 hours, followed by a slower infusion over the next 22 hours, is being planned for the intravenous therapy. Active computation is going to help work out the optimal dosing schedule.
Investigator Christopher Barrett says, "If effective and safe for the treatment of ARDS in patients with COVID-19, tPA could save lives by reducing recovery time and freeing up more ventilators for other patients in need."
Senior author Michael B. Yaffe, suspects that "patients with aggressive clotting will show the most benefit from tPA treatment, and this new clinical trial will reveal whether that's the case." If so, the ready availability of the drug in every major hospital will make it possible to save many lives immediately.
What will the trial mean?
The results of the clinical trial for tPA are awaited by physicians across the country, who face an alarming shortage of resources as hospitals fill up. Since tPA is FDA-approved and widely available across the country, doctors will be able to prescribe it for use in COVID-19 induced ARDS once it is proven to be safe and effective.
The research team has already started enrolling patients with COVID-19 induced ARDS admitted to BIDMC in the clinical trial. Blood levels of clotting factors and other characteristics will be measured to identify which patients fit the criteria for the use of the drug, according to Yaffe.
The research collaborates with Beth Israel Lahey Health COVID-19 Innovation Hub - an incubator led by Chief Academic Officer of Beth Israel Lahey Health, Gyongyi Szabo, MD, Ph.D., which is exploring unforeseen medical challenges as the country fights the public health emergency.
Journal reference:
Is There a Role for Tissue Plasminogen Activator (tPA) as a Novel Treatment for Refractory COVID-19 Associated Acute Respiratory Distress Syndrome (ARDS)? Moore, Hunter B., Barrett, Christopher D., Moore, Ernest E., McIntyre, Robert, Moore, Peter, Talmor, Daniel S., Moore, Frederick A., Yaffe, Michael B., Journal of Trauma and Acute Care Surgery: March 20, 2020 - doi: 10.1097/TA.0000000000002694, https://journals.lww.com/jtrauma/Citation/publishahead/Is_There_a_Role_for_Tissue_Plasminogen_Activator.97967.aspx