The world is now at a standstill, as many countries have imposed restrictions to stem the spread of the coronavirus disease (COVID-19). Nations are in lockdowns indefinitely, until the situation improves. The vast spread of the novel coronavirus is now inevitable, as the number of confirmed cases topped 1.85 million, many scientists are determining health measures that could help mitigate the global pandemic.
A new modeling paper shows that dynamic physical distancing and other measures could help maintain health system capacity. It can also reduce intensive care units (ICUs) admissions, preventing them from becoming overwhelmed due to COVID-19. The good news is, the new model shows this physical distancing done while allowing for periodic psychological and economic breaks from the restrictions.
Published in the Canadian Medical Association Journal (CMAJ), the study focuses on physical distancing interventions used in Canada to slow the spread of SARS-CoV-2, or the severe acute respiratory syndrome coronavirus 2, the causative agent of COVID-19 disease. The researchers studied how various nonpharmaceutical interventions could help control the global pandemic, ravaging the world today.

People standing waiting in line far apart to maintain social distance distancing during COVID-19 coronavirus outbreak with mark cross signs on sidewalk pavement by grocery food store. Image Credit: Kristi Blokhin
Model of COVID-19 transmission
To arrive at their findings, the researchers from the Dalla Lana School of Public Health, University of Toronto, used an age-structured compartmental model of COVID-19 transmission in the population of Ontario, Canada.
The team compared the base case with limited testing, isolation, and quarantine to other measures, such as enhanced case finding, restrictive physical-distancing measures, or a combination of less restrictive physical distancing and enhanced case finding.
Further, the team modeled strategies to help 'flatten the curve' and reduce the burden on the health system. The interventions were either implemented for fixed durations or dynamically cycled on and off, based on the availability of ICU beds.
Study estimates
For the base case, they found that with limited testing, isolation, and quarantine measures, and with about 56 percent of the population becoming infected, there would be around 107,000 hospital admissions and 55,000 cases in Intensive Care Units (ICUs) at the peak of the pandemic.
The team also found that using physical distancing and contact tracing for 12 to 18 months would substantially reduce the number of people infected, with varying results depending on how aggressive the implemented physical distancing measures were.
Implementing dynamic response interventions, which involves the cycling of on and off interventions, is an effective way to reduce the proportion of the population affected at the end of two years. The measures include social distancing, which can be eased to provide periods intended for economic and psychological relief. The measure is useful because when the team calculated the intervention being implemented by about 13 months, the average overall attack rate decreased by 2 percent.
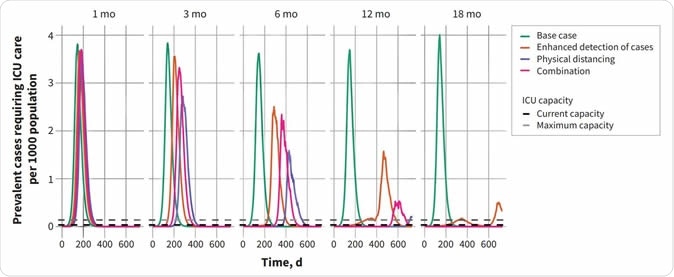
Projected intensive care unit (ICU) bed requirements and attack rates for fixed-duration interventions. (A) Prevalent cases requiring intensive care are shown for intervention durations of 1, 3, 6, 12 and 18 months. Maximum and current ICU capacity in Ontario are indicated by the dashed horizontal lines. Median values are presented. (B) Model-projected percentage of the population infected over the 2-year period. Attack rates include all infections, regardless of severity.
"Physical distancing and other public health measures can reduce COVID-19 spread, but once these measures are lifted, we're at risk of an uptick in cases," Dr. Ashleigh Tuite, assistant professor of epidemiology at the Dalla Lana School of Public Health, University of Toronto, said.
"Dynamic response measures that can be turned up and down in response to where we are on the epidemic curve provide a way to curb transmission while also providing periodic breaks and a chance to return to a more normal life," she added.
The researchers believe that there will be expected ups and downs with dynamic interventions. With the new model developed, they showed that countries could modulate response measures to avoid overwhelming the health care system while attempting to reduce the adverse effects of measures on the economy and society.
The researchers project that dynamic physical distancing that reacts to changes in ICU occupancy could maintain health system capacity and also allow periodic psychological and economic respite for populations.
"Repeated outbreaks of COVID-19 will most likely occur because of the reintroduction of infection from other countries until a vaccine is developed or we develop herd immunity in which much of the population has developed antibodies to the virus," Dr. David Fisman, professor of epidemiology at the Dalla Lana School of Public Health, said.
Source:
Tuite, A., Fisman, D., and Greer, A. (2020). Mathematical modeling of COVID-19 transmission and mitigation strategies in the population of Ontario, Canada. CMAJ. https://www.cmaj.ca/content/cmaj/early/2020/04/08/cmaj.200476.full.pdf
Journal reference:
Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) - https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6