The risk of getting infected with COVID-19 disease is higher among healthcare workers who are in close contact with infected patients
A higher viral infective dose or more viruses a person comes in contact with can result in a higher risk of infection, and in some cases, the infection may be more severe compared to others. Studies have shown the same to be true for other viral infections such as influenza. An American study has also revealed that healthy volunteers exposed to a higher number of influenza viruses are at risk of worse symptoms compared to those who are not exposed.
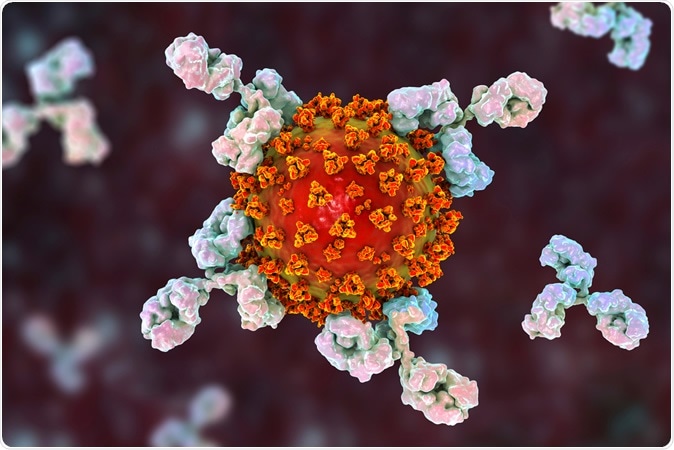
Antibodies attacking SARS-CoV-2 virus, the conceptual 3D illustration for COVID-19 treatment, diagnosis and prevention. Image Credit: Kateryna Kon / Shutterstock
Why does it happen?
This, speculate experts, could be due to the higher number of viruses starting the infection and thus infecting more cells at the start of the disease process. A single cell infected by a virus becomes a virus factory and produced numerous viruses at the end of which the cell bursts open, releasing the daughter viruses into the body. Consequently, if more cells are affected at the start of it all, it can cause more severe disease. Even a small number of viruses can produce an infection, but the symptoms may be milder. Previous research has shown the norovirus infection that leads to vomiting and diarrhea can occur with just 18 viral particles
How does this relate to COVID-19?
The virus causing COVID-19 disease, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is highly infectious, and the initial dose could be related to the severity of the infection. Researchers say that the load of the virus in the aerosols that lead to the infection and its proportionate effects on the severity of the disease can be determined only by “experimental challenge studies.” This means infecting healthy volunteers deliberately, which is ethically not permissible.
How can the viral load be determined?
According to researchers, viral load or the level of infective particles that cause the infection could be determined by a quantitative test or the standard international test. A load result between 0 and 40 can be obtained, and this is called the Ct value or threshold cycle.
If the Ct value is low (say 15), the levels of virus in the sample is said to be very high. If a sample has Ct of over 35, the viral load is low. The level of Ct correlates to disease severity.
What do we know?
At present, there are small and conflicting reports regarding the correlation between viral load and disease severity. Some studies have also suggested that the body’s response to the virus is critical in determining the effects of the infection, as is the immune response and immune status of the patient and comorbidities. If the immune system is not activated, the virus multiplies faster, and if the immune system is overtly activated, it can lead to damage to other tissues by causes the cytokine storm.
Comorbidities such as high blood pressure, asthma, diabetes, and renal disease can also raise the risk of severity of the infection.
Understanding COVID-19: what does viral RNA load really mean?
A recent study published in the latest issue of The Lancet Infectious Diseases looked at the viralRNA load in patients. The study was titled, “Understanding COVID-19: what does viralRNA load really mean?”
The researchers state that earlier studies with MERS and SARS have not clearly shown a “relationship between individual patient clinical course and viral RNA load.” This study with COVID-19 patients, they write, shows up three distinct clinical courses of the disease. From their review of available literature, the team says that “patients with COVID-19 with more severe disease requiring intensive care unit admission had high viral RNA loads at 10 days and beyond, after symptom onset”. Some patients, they wrote had low viral loads in nasopharyngeal secretions but still had a worsening clinical course. This could be due to the immunological manifestations more than the viral load, feel the researchers.
They explain that the risk of transmission is higher from people who had fewer symptoms and more viral load in their nasopharyngeal samples. They write, “Individuals within the community, policymakers, and frontline healthcare providers, especially general and emergency room practitioners, should be alert and prepared to manage this risk.”
SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients
In another letter to the editor of the New England Journal of Medicine, a group of researchers explored the viral load in infected patients. The title of their research letter is “SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients.”
The team wrote that the transmission of the virus “occurred mainly after days of illness and was associated with modest viral loads in the respiratory tract early in the illness, with viral loads peaking approximately ten days after symptom onset”. They wrote that they tried to quantify the viral load in the nasal and throat swabs of symptomatic patients. They added, “Higher viral loads (inversely related to Ct value) were detected soon after symptom onset, with higher viral loads detected in the nose than in the throat.” Symptomatic and asymptomatic patients had similar viral loads.
Journal references:
- Matthew J. Memoli, Lindsay Czajkowski, Susan Reed, Rani Athota, Tyler Bristol, Kathleen Proudfoot, Sarah Fargis, Matthew Stein, Rebecca L. Dunfee, Pamela A. Shaw, Richard T. Davey, Jeffery K. Taubenberger, Validation of the Wild-type Influenza A Human Challenge Model H1N1pdMIST: An A(H1N1)pdm09 Dose-Finding Investigational New Drug Study, Clinical Infectious Diseases, Volume 60, Issue 5, 1 March 2015, Pages 693–702, https://doi.org/10.1093/cid/ciu924
- Understanding COVID-19: what does viral RNA load really mean? Joynt, Gavin M et al. The Lancet Infectious Diseases, https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30237-1/fulltext
- SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients, N Engl J Med 2020; 382:1177-1179 DOI: 10.1056/NEJMc2001737, https://www.nejm.org/doi/full/10.1056/NEJMc2001737