Even as the COVID-19 outbreak continues to cost lives and cause tremendous sickness in almost every country of the world, scientists are grappling with a lack of information as to what causes the virus to thrive and how they can block its spread.
The current study aims at finding a causal association between vitamin D levels and COVID-19 outcomes, taking into account the observed link between the geographical location above the tropical latitudes with the severity of illness. The researchers also model the vitamin D-pandemic relationship in two ways. Finally, they analyze how the mechanisms of disease in COVID-19 involve vitamin D and how they can be used to mitigate the severity of the condition.
The most severe outbreaks of COVID-19 have been associated with higher latitudes above 30oN. Global reports reveal that the spread of the virus and the fatalities are significantly related to the latitude of the region.
In the past, outbreaks of coronaviruses and influenza viruses have followed a markedly seasonal trend. Seasons are, of course, related to the latitudes, and this helps explain some of this variation.
Winter transmission is higher with enveloped viruses like the coronaviruses because they are more easily destroyed by heat and by ultraviolet radiation than other viruses. However, this doesn’t account for the higher fatality rates at higher latitudes.
Vitamin D is involved in calcium metabolism but also in regulating the immune system. Since vitamin D is produced in the skin by a sunlight-activated process, deficiency can occur seasonally in the temperate zones.
Low vitamin D levels are associated with old age, dark skin, low levels of sunlight exposure, dietary deficiency, and non-fortified foods. Italy, the European country, which experienced the most significant number of severe and fatal COVID-19 cases, also has the highest levels of vitamin D deficiency.
How was the study done?
The researchers, independent doctors, gathered data on COVID-19 cases, recoveries and deaths from the John Hopkins public repository, and latitude-based population data from the Center for International Earth Science Information Network, Columbia University.
The fatalities due to the illness were analyzed by latitude up to March 28, 2020, by putting the total number of deaths for each location into separate data sets spanning 5 degrees of latitude each, from 40 oN to 70 oN. This was used to calculate the deaths per million at each increment of latitude.
The severity of illness was also compared with the timeline of global viral spread, to determine if the timing of infection onset plays a role in the severity of the outbreak.
The next step was to analyze the severity by location for almost 240 locations where cases were reported, looking at the ratio of recoveries to deaths, as well as the total fatality count. They also assessed the Epidemic Severity Index (ESI), comparing the severity to a reference hospital survival ratio S, which is about twice the severity of the seasonal flu in the US.
The ESI scores are plotted both linearly and logarithmically. The linear plot shows the total number of deaths, while the log form shows locations that have minimal ESI values that escape the linear graph.
Locations at which cases were reported within the first six weeks of the first Wuhan outbreak are examined in-depth, and outliers are identified.
Modeling with causal and noncausal frameworks
Using a formal causal inference (CI) framework, they plotted directed acyclic graphs (DAGs) to find causal relationships. The large-scale pandemic makes it easy to use such models with multiple, distinct, and independent input variables. These allow for qualitative analysis, with the generation of predictions that can be compared with observed data to arrive at strong causal conclusions.
More conventional CI models quantify the strength of a causal relationship through a single model. The current model is aimed at identifying a causal relationship by creating two opposing models to express the two contrasting answers to the hypothesis. This results in testable predictions that can be compared with observations to test the fit of the model.
Exogenous variables fall into three categories: sources of vitamin D, causes of vitamin D deficiency and causes of disease unrelated to vitamin D. Illnesses are also classified the same way as those that reduce vitamin D, those that are caused by or worsened by vitamin D deficiency, and those which are unrelated to vitamin D levels.
After adjusting for biases and confounders, the predictions generated by both models were tested, and the differences tabulated. These were then compared with the available observations.
What did the study show?
The researchers found several interesting observations that support the causal hypothesis.
Latitude-linked differences in severity
All severe outbreaks causing large numbers of deaths (3% to 37%) have occurred above +30ºN latitude, in winter locations, for an average fatality of 11% for latitudes from 30ºN to 55ºN.
Outbreaks in tropical and southern hemisphere countries were mild, with a fatality rate of 0.2% per million. This cannot be due to the timing of the outbreaks, which also occurred in 35 Asian locations near China within 14 days of the start of systematic reporting on January 22, 2020. Spreading across international boundaries, the pandemic affected most other places within the next three weeks.
ESI by location
The peak ESI scores showed that 9 locations had severe outbreaks scores over 2.5, and all were at latitudes above 30°N. Above this line, the timeline correlates with severity, but not below it. In other words, more southern locations had many outbreaks, but none became severe.
Vitamin D deficiency
Italy has among the highest rates of hypovitaminosis D and COVID-19 severity. Women between 60-80 years have low vitamin D levels in up to 76% of cases, as well as 82% of patients enrolled in various rehabilitation programs for neurological-based deficits.
Outlier locations
Canada, Germany, Japan, and South Korea are outlier locations above 35°N, but with mild severities up to April 28, 2020. All have adequate vitamin D levels, on average.
On the other hand, Iran had a severe outbreak though it is at a sunny latitude of 31°N to 32°N, while Israel, though in the same latitude, had fewer deaths. However, Iran has a very high prevalence of vitamin D deficiency but not Israel.
Again, Brazil and the Philippines are outliers in the region below 30°N. Both are known to have very high levels of vitamin D deficiency and also large populations of mixed-origin and Black people.
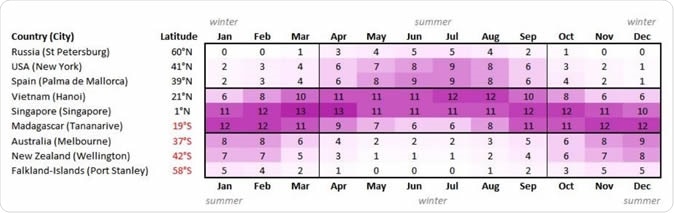
Maximum UV Index by month and latitude
Vitamin D deficiency could increase the severity of COVID-19
The researchers found that many of the predictions of the causal model match the observed data. For instance:
- Severe outbreaks and high case-fatality rates in the northern hemisphere winter locations only
- Tropical and southern latitudes have mild outbreaks even without quarantine or isolation measures
- Outliers in the northern latitudes have high vitamin D levels and less severe outbreaks
- Outliers in the southern latitudes have very large proportions of severe vitamin D deficiency and so more severe outbreaks
- Pregnancy and infancy are very unexpectedly not at risk in the developed countries of the northern latitudes because of routine supplementation with vitamin D
- Communities with dark skin in both the US and the UK (winter hemisphere locations) have double the average case fatality rates
- Factors that inhibit or lower vitamin D levels such as older age, the use of sunblock, certain medical conditions and behaviors (like sunlight avoidance or constant use of full-body clothing), dietary deficiency or certain drugs, were observed to increase the case fatality rate even in low-latitude locations
The second noncausal model, which assumes that vitamin D is not a cause for severe COVID-19, predicts:
- No latitude-case fatality rate correlation
- Winter locations will show lower rates of spread only in the presence of quarantine, isolation and social distancing
- Adequate vitamin D levels and high intakes of fish at winter locations will not be linked to lower fatalities
- Pregnancy and infancy will be high risk despite routine vitamin D supplementation
- Factors like older age, sunblock use and other behaviors or conditions which reduce vitamin D levels will not show correlation with case fatality rates in healthy people
- Case fatality rates will show a correlation with other illnesses only if they are unrelated to vitamin D, after accounting for confounding factors
The historical lesson
Historical supporting data include the fact that the Spanish flu pandemic, which caused 50-100 million deaths, occurred at a time when low vitamin D levels were found in 80% to 90% of children in northern Europe and the north-eastern US. Sunshine and fresh air were advised, and were the only effective therapies, for reasons then unknown.
After vitamin D was confirmed to exist in 1925 and to be anti-rachitic, food fortification with vitamin D became common, leading to the eradication of low vitamin D levels. However, high calcium levels led to the prohibition of vitamin D addition in many European countries in the 1950s.
The levels of vitamin D fell again and became worse as sunscreen creams with ultraviolet-absorbing compounds came into use in the 1970s.
It is interesting that the only period when there were no epidemics and no new flu strains were the 37-year period between 1920 and 1957, which is the only time in history when large-scale vitamin D supplementation occurred.
Biochemical mechanism of severe illness and mortality in vitamin D deficiency
Vitamin D deficiency is present in 90% of patients with acute respiratory distress syndrome and is linked to a poor outcome. Chronic deficiency of vitamin D activates the renin-angiotensin system and causes lung fibrosis. It is also linked to cardiovascular disease, diabetes, and dementia.
COVID-19 causes injury to the heart muscle as well as long-term cardiovascular damage so that it is sure to increase the number of deaths in patients who already have such underlying conditions.
Vitamin D restores the balance of the RAS and reduces the severity of the lung injury by inhibiting the RAS-activation-mediated cascade of inflammation. It also dampens the innate immune response starting with dendritic cell inhibition and enhances anti-inflammatory cytokine production.
At least in severely ill patients with deficient vitamin D levels, high oral doses of vitamin D reduce the mortality rates.
Some recent studies show that vitamin D deficiency increases deaths from all causes and from cancer, even without reducing the incidence. The benefits are difficult to demonstrate because vitamin D supplementation takes days or weeks to show a positive effect on inflammatory and immune responses.
The study concludes: “Recent and historical data are highly consistent with a causal protective role for Vitamin D in respiratory disease risk and especially in the case of COVID-19. By contrast, the same evidence conflicts with predictions made by an acausal/bystander model.”
While the study design is good, the effect size can be quantified only through larger data sets. However, vitamin D supplementation is an inexpensive yet effective way to confer protection against seasonal respiratory diseases, and also against the COVID-19 pandemic.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.