The current pandemic caused by the SARS-CoV-2 virus began in the Chinese city of Wuhan in the last month of 2019, but spread rapidly, first within the city and then the country, and finally to the rest of the world, within four months. It has now affected almost 187 countries and territories, with 4 million-plus reported cases and over 282,000 dead.
This respiratory illness spreads with ease between people, mainly through direct contact and droplets from the respiratory tract. However, it has been found in fecal samples as well.
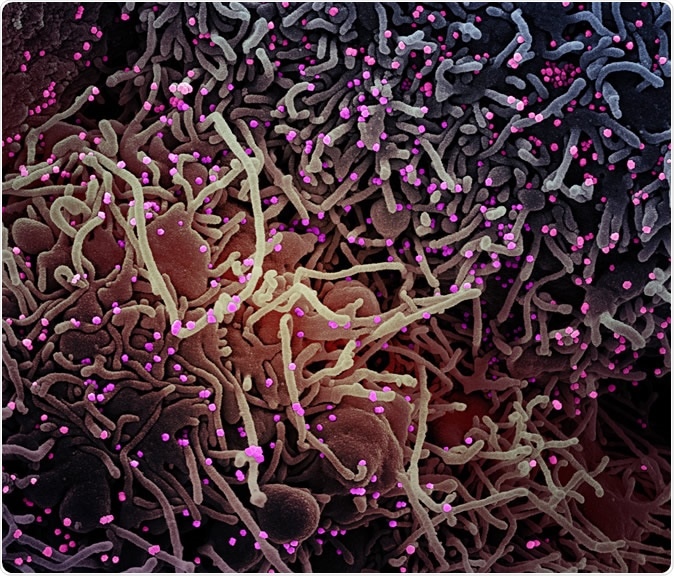
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of a VERO E6 cell (purple) exhibiting elongated cell projections and signs of apoptosis, after infection with SARS-COV-2 virus particles (pink), which were isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
How Was the Study Done?
The present study aims to find out how long fecal samples remain positive for the virus and whether the virus can be spread through feces. This is of great public health importance as it could modify the duration of quarantine, prevention of spread, and the duration of the treatment period.
The current study focused on the clinical details of seventeen COVID-19 patients in a retrospective single-center design covering the period January 22 to February 7, 2020. The national criteria then in place for the diagnosis of COVID-19 were used to confirm the cases. All patients tested positive for the viral nucleic acid by quantitative real-time PCR (qRT-PCR) on pharyngeal swab samples.
The patient was deemed negative (SARS-CoV-2 free) when three successive pharyngeal swabs were negative on qRT-PCR at intervals of at least 24 hours each. A negative fecal swab was defined as two successive fecal samples negative by the same test at 24 hours or more apart.
The clinical, laboratory, and chest imaging (CT) records were reviewed for all patients. Two of the patients had severe symptoms, but no patients died.
What Were the Findings?
The researchers found that all the patients had been exposed to known cases or had been to high-risk locations. Two of them had hypertension. The average incubation period was 5.5 days.
Fever was present in all patients, followed by dry cough in 7 patients, other symptoms including sputum, headache, and muscle pain being uncommon.
All patients received antiviral drugs and five required oxygen support by nasal catheter. Fourteen of them received antibiotics, and 4 of them were on hormones.
Fecal samples turned out positive for the virus in 11 patients, or 65%, remaining positive for 17 days on average (most prolonged duration 40 days). This was markedly longer than for the pharyngeal swab samples in 16 of 17 patients.
The clinical features of all patients in the study were similar, regardless of whether the virus was shed through the feces or not. Gastrointestinal manifestations like diarrhea, nausea, or vomiting were uncommon. The fecal carriage was not significantly correlated with such symptoms. However, it should be noted that later studies have shown that some patients present with gut-related features as their primary complaint.
The virus is an enveloped single-stranded RNA coronavirus, binding to the angiotensin-converting enzyme 2 (ACE2), which is prominently found on type II alveolar epithelial cells in the lung, in the esophageal epithelium, and in the intestinal epithelium. The virus has also been cultured from these samples.
This raised the question of whether the infection could be transmitted by the fecal-oral route.
Findings and limitations
The patients were investigated for epidemiological parameters. Six of them belonged to two families, of which three from one and two from another were positive, while the sixth was negative.
All of them lived in different houses and had good personal hygiene before they became sick. This ruled out the fecal-oral route and rather indicated droplet or direct contact transmission.
After discharge, no family members living in the same households were infected, as ascertained by follow-up. The sample size is small, however, and the follow-up period short, so that firm conclusion cannot be drawn.
Other potential confounders could be the risk of false-negative PCR tests of both types of samples; the lack of daily fecal sampling which may have introduced error into the observed duration of virus passage in feces in some patients; and the absence of data on viral testing of alveolar lavage fluid.
There were only two patients with severe disease in this sample, making it impossible to correlate fecal viral passage with the severity of the disease.
Feco-oral transmission unlikely
The researchers say they did not identify evidence for fecal-oral transmission of COVID-19. However, they say, since fecal samples remain positive for the virus for a significantly longer time compared to upper respiratory samples, disinfection and isolation should be carried out meticulously throughout the recovery period of such patients to avoid contamination of the surroundings.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.