Effective drug development must streamline the number of candidate drugs that enter the cycle, to bring down the cost and the time of the process. Recent studies recommend integrating a variety of techniques to develop pipelines for research and development (R&D) as well as using genetic data to identify the most likely successful new drugs. Proteomics and transcriptomics are among the most valuable fields towards this end.
At present, there are over 150 clinical trials testing drugs that are thought to be possibly effective in boosting the survival and improving the recovery of COVID-19 patients. These include hydroxychloroquine, chloroquine, and baricitinib.
Another route of gathering evidence on potentially useful drugs against COVID-19 is by finding the host proteins that facilitate viral entry and infection, and by examining the possibility of repurposing earlier drug targets in the SARS-CoV to combat the current virus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
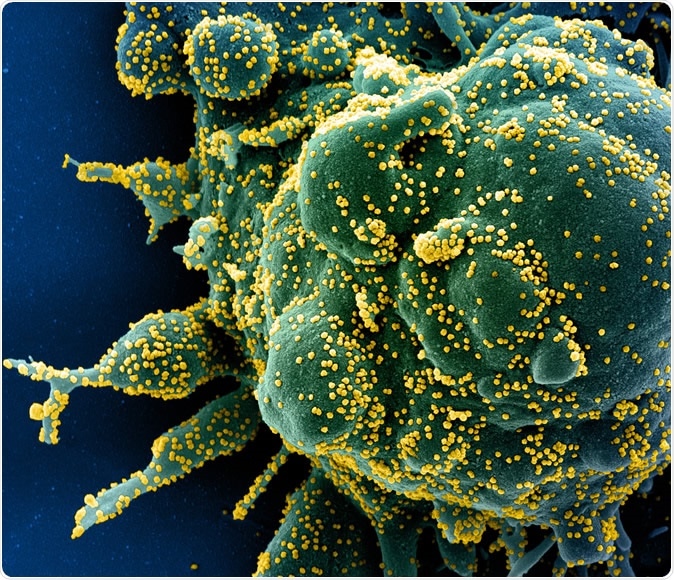
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of an apoptotic cell (green) heavily infected with SARS-COV-2 virus particles (yellow), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Utility of this Approach
A recent study found over 330 human host proteins that are necessary for the virus to infect humans. These interact with 26 viral proteins. This could help advance R&D along the first route.
The second method has been used by a few studies, which have yielded 59 mouse genes that are linked to the earlier SARS-CoV infection. Among these, there are 44 that have equivalents in the human genome. By blocking viral-human protein interactions, it may be possible to target viral infection mechanisms more effectively with a lower chance of drug resistance, compared to directly targeting the virus.
A primary issue with this approach is the danger of inadvertently producing other effects that could worsen complex disease conditions – or even benefit them. The current study is aimed at evaluating how these drug targets could affect the human body’s functioning, based on an understanding of the underlying genetics.
The Actual Study?
The researchers used the protocol for drug prioritization, which they successfully developed earlier, to test 353 drug targets that possibly interact with the virus. They wanted to observe how these drugs caused other outwardly discernible effects of the infection, as well as how they achieved both intended and unintended effects on complex diseases.
They first constructed a disease atlas displaying the human proteins and genes that take part in viral entry. This was via Mendelian randomization studies, providing over 372,000 unique predictions of how the drug affects a disease. This was based on plasma proteomics as well as tissue-specific transcriptomics.
As a result, they were able to evaluate how these 353 potential drugs might act in 49 phenotypes of viral infection, how they could affect over 500 complex diseases, and change 72 phenotypes of disease. These results were assessed with respect to data from drug trials, as well as the druggable genome, to identify the top drugs with the highest possibility for repurposing, and the least side effects.
They have created an online open-access platform that contains the results of all the tests, so as to allow anyone to examine the results for any of the drugs rapidly.
What Did the Study Show?
The atlas of drug target-disease interactions provides over 370,000 target-disease associations in 11 tissues that are relevant in the COVID-19 scenario. Of them, 833 had strong evidence from MR imaging of the 11 tissues. 726 of these also showed robust colocalization, for a colocalization probability of over 70%. These were the study’s most robust findings.
The importance of detecting such associations is the ability to carry out analyses of how the expression of certain targets affects specific diseases, depending on the tissue. For instance, the effects of the drug targets on Crohn’s disease, hypertension, atopic disorders, and diabetes could be assessed. Anywhere from 11-17 of the target genes had associations with these four diseases, based on which tissue was studied.
Secondly, the drug targets were analyzed for association with 49 viral infection phenotypes. There were two strong associations, namely, the NEU1 gene with chronic hepatitis and the DPY19L1 gene with viral enteritis. There were also three less strong but suggestive associations, like the JAK2 gene with chronic hepatitis.
Thirdly, the study showed 45 potential ways in which the proteins could affect disease traits and 430 similar associations with the mRNA expression. Among these, there was 95 target associated with 105 diseases or disease expressions. The JAK2 gene, for instance, is associated with nine disease phenotypes, ranging from atopy to obesity, which suggests potentially pleiotropic actions for this gene.
Finally, they found 249 associations where the drug target affected a disease phenotype differently depending on the tissue analyzed. Among these were 52 unique genes expressed in 7 tissues to affect 47 unique diseases.
There were 29 strongly associated tissue-dependent effects of the drug target on the disease in more than a single tissue, among which only two failed to show the same direction of effect when expressed in blood as well as a range of other tissues.
For instance, the DHODH gene affects low-density lipoprotein cholesterol (LDL). A drug being marketed against high LDL, called Leflunomide, works by inhibiting this gene. Leflunomide is also being considered as a COVID-19 therapy.
The analysis showed that this drug is expressed only in relation to LDL without many other diverse actions, over a broad spectrum of tissues from the lung to colon.
Prioritizing Drug Targets
The researchers scored the 726 associations found by MR between target and disease, using clinical trial data as well as the putative evidence that they caused different phenotypic effects across a range of tissues, to come up with the most druggable associations. 499 of them were unique pairings of target and disease, with the others being observed in more than one tissue.
They set up four scoring classes, such as the omics score, the trial score, the druggability score, and the infection score. Each score was scaled from 1 to 100. There were high scores for 2 of the 499 associations in 3 of 4 classes, which made them the targets with the highest development priority. 77 scored high in two classes and 97 in one. The remaining 323 had universally low scores and are therefore considered the lowest priority drug targets.
Some targets include the ITGB5 gene that is targeted by the drug Cilengitide, which was intended for glioblastomas and similar tumors. Its high scores and the genetic profile suggest it has the potential to reduce the high blood pressure. Among the top 5, all lacked strong associations with conditions like cardiac arrhythmias, which could affect their use in COVID-19.
On the other hand, the TLR9 gene, which is targeted by the drug hydroxychloroquine has high scores in two categories but a low score for the other two. No clinical evidence has yet accrued as to the antiviral or clinical benefit from a combination of this drug with azithromycin. Moreover, this gene may increase the chance of embolic stroke, asthma, and certain immune conditions.
The Advantages of This Approach
The study was able to promote the prioritization of drug targets in three ways: examining the safety issues that may arise from repurposing drugs for COVID-19 treatment; identifying promising drug targets; and finding how the drug target affects the human phenome in different tissues.
Using this approach, a potential drug, Baricitinib, is being tested for its effectiveness in COVID-19. It is thought to inhibit the JAK2 protein, and thus reduce systemic inflammation. However, the current study proposed that it could also cause chronic hepatitis. In fact, the literature suggests that hepatitis B is reactivated after treatment with JAK 2 inhibitor ruxolitinib.
The three high-potential drugs from this study include immunosuppressive drug Leflunomide, used in rheumatoid arthritis, among other conditions, and Cilengitide. The former has antiviral activity against multiple viruses, and the current study also suggests it has lipid-lowering properties, while the latter has antihypertensive activity, possibly.
Finally, some of these targets are expressed in multiple tissues to produce the same phenotype, but others show changing expression specific to the tissue.
While some limitations exist, the study does provide a pipeline for statistical genetics study and an open-access platform to arrange drug targets against COVID-19 in order of priority. Genome-wide association studies (GWAS) could further improve the quality of the data, making it still more useful in finding promising drug targets among potentially repurposed drugs.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources