The ongoing COVID-19 outbreak has caused more than 4 million cases and nearly 300,000 deaths. Patients who already have high blood pressure, heart disease, respiratory disease, or cancer are known to have worse outcomes than those without these conditions. However, other concurrent conditions have been less studied.
Assessing Outcomes In COVID-19 and HIV Coinfection
The current study examines the effect of COVID-19 on individuals with HIV, who number almost 40 million worldwide. This was a retrospective study involving all patients admitted with COVID-19 at acute care hospitals within the NYU Langone Health System.
All patients in the study had tested positive for the illness, were hospitalized in one of the study centers, and had either been discharged, transferred to hospice care or died at the time of the study. Those who were still in hospital were not included.
The researchers collected demographic details, examined the past medical history, admission data, and laboratory results, as well as the hospital outcomes.
Twenty-one patients were HIV-positive, and over 2,600 patients who were not. Of the non-HIV patients, 42 were selected as matched controls using admission date, age, body mass index, gender, history of tobacco use, chronic kidney disease, high blood pressure, asthma, chronic obstructive lung disease, and heart failure as the criteria.
What were the findings in HIV/COVID-19 patients?
Upon analysis of the two groups of patients, the researchers found that 19 of the 21 HIV patients with COVID-19 had CD4 counts measured, and 17 had viral load measured, on or before the day of admission. The median CD4 count at this time was 298/uL, with only 6/19 having counts below 200/uL.
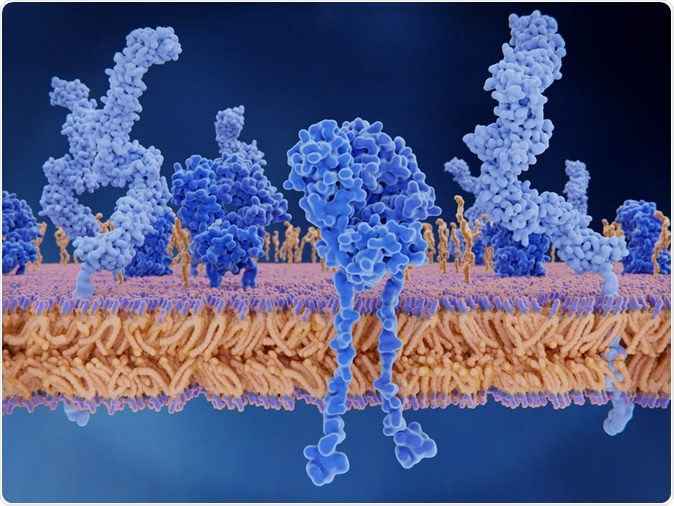
The T-cell receptor activates the immune response to antigens in T-lymphocytes. T-cell receptors (dark blue), CD4 molecules (light blue), glycolipids (orange). 3d rendering. Iluustration Credit: Juan Gaertner / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The viral load was less than 50 copies/mL in 15/17 patients. All HIV patients were on highly active antiretroviral therapy (HAART) before admission.
There was no significant difference in the laboratory results that reflected the white cell count, hemoglobin, ferritin, D-dimer, troponin, CPK, and others, which related to the severity of infection and organ damage. The absolute lymphocyte count and C-reactive protein levels were higher in HIV patients than in the controls.
The percentage of patients with abnormal chest imaging results, such as consolidation, infiltration, or opacities, was higher in the HIV cohort compared to non-HIV patients, at 91% and 64%, respectively. If the presence of consolidation, opacity or infiltrate at any time during hospitalization was analyzed; however, the two groups were comparable.
Peak CRP values were higher in HIV patients, at 185, vs. non-HIV, at 128. This did not predict higher mortality, however, in this group. Complications like acute cardiovascular events (heart attacks, strokes, deep vein thrombosis, and pulmonary embolism) were uncommon in both groups (1/21 vs. 1/42 patients had a combined pulmonary embolism and heart attack).
How Were Outcome Measures Different in HIV Patients?
There was no significant statistical difference in duration of hospital stay, ICU admission, mechanical ventilation, transfer to hospice, or mortality, between the two groups. Neither was there a greater use of supplemental oxygen in the HIV group. With both these measures, however, there was a trend towards the upper side in the HIV cohort.
Twelve patients in all had suspected bacterial superinfection of the lungs, for which sputum cultures were performed. These comprised six from each group. Altogether, 4/12 cultures were positive, of which 3 came from the HIV cohort – two with polymicrobial infections. All four culture-positive patients died in hospital despite antibiotic therapy, six or more days after the clinical diagnosis of suspected superimposed pneumonia was made.
The researchers suggest that based on the current study, HIV-positivity does not cause a significant clinical impact on the course of COVID-19.
Non-Significant Trends
Some trends were detected, suggesting that these patients might have worse outcomes since more patients in the HIV cohort needed intensive care unit (ICU) admission, required mechanical ventilation, died, or were moved to hospice care.
Mechanical ventilation was needed in 24% and 12% of the HIV and non-HIV cohorts, respectively, while the death rate was 29% and 23%, respectively. Compared to the overall statistics - 28% and 19%, respectively – from all patients in this hospital system, the need for ventilation is lower, but the mortality is higher in both cohorts than expected. However, international mortality rates do range from over 21% to 28%, making this a non-significant variation.
Other notable findings include a persistent trend towards higher chances of chest imaging abnormalities, throughout the course of hospitalization. The chest X-ray at admission was not a good indicator of the severity of illness, as has been reported before in more extensive and more general studies.
Four patients had superimposed bacterial pneumonia, of which 3 came from the HIV cohort. It is already known that HIV patients have a higher chance of bacterial pneumonia and other bacterial infections, compared to the general population. HIV patients at risk for severe bacterial infection have risk factors such as immunosuppression, cancer, and diabetes – all of which are already linked to poorer outcomes in COVID-19.
Implications for Care Of HIV/COVID-19 Patients
The observation that all the HIV patients with superimposed pneumonia died may be important in guiding clinical decision-making in these patients. However, the small sample size precludes making any conclusions about the association of mortality with such infections. This analysis, as well as the possible link between COVID-19 and secondary bacterial infection in HIV patients, is reserved for future more extensive studies.
Since all the patients in this study were already on HAART and were mostly well-controlled, these findings may not apply to HIV patients with high viral loads, low CD4 cell counts, or who are not on treatment. Other confounding factors may have played a role due to the retrospective design. However, the findings serve to indicate that HIV patients may have outcomes comparable to non-HIV patients with COVID-19 infection if they are otherwise matched.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Karmen-Tuohy, S. et al. (2020). Outcomes among HIV-positive patients hospitalized with COVID-19. medRxiv preprint. doi: https://doi.org/10.1101/2020.05.07.20094797. https://www.medrxiv.org/content/10.1101/2020.05.07.20094797v1
- Peer reviewed and published scientific report.
Karmen-Tuohy, Savannah, Philip M. Carlucci, Fainareti N. Zervou, Ioannis M. Zacharioudakis, Gabriel Rebick, Elizabeth Klein, Jenna Reich, Simon Jones, and Joseph Rahimian. 2020. “Outcomes among HIV-Positive Patients Hospitalized with COVID-19.” Journal of Acquired Immune Deficiency Syndromes (1999), June. https://doi.org/10.1097/QAI.0000000000002423. https://journals.lww.com/jaids/Fulltext/2020/09010/Outcomes_Among_HIV_Positive_Patients_Hospitalized.2.aspx.