Researchers in the Netherlands, Cuba, and Italy have made important discoveries about the carbohydrate-mediated binding of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike protein to host cell lectin receptors and host lung microbiota.
The findings point to new molecular pathways involved in SARS-CoV-2 infection, independent of angiotensin-converting enzyme 2 (ACE2) binding, that use host lectins and signaling to aid viral infection and exacerbate the host immune response.
This novel, previously unreported finding could lead to the design of new approaches to treating bacterial infections in patients with COVID-19, say Fabrizio Chiodo (Amsterdam UMC, The Netherlands) and colleagues.
A pre-print version of the article can be accessed in bioRxiv*, while the article undergoes peer review.
“New and unexplored angles”
“The immediate call for translational research in the field of coronavirus disease (COVID-19) pandemic needs new and unexplored angles to support and contribute to this important worldwide health problem,” say Chiodo and team.
The SARS-CoV-2 that causes COVID-19 accesses host cells using a glycosylated spike protein to bind to the ACE2 receptor. Still, during the first steps of infection, other carbohydrate-mediated host-pathogen interactions may play important roles, as has previously been shown for HIV-1, influenza, and SARS-CoV, amongst others.
Glycosylated viral proteins are recognized by various host carbohydrate-binding receptors, which induce immune responses that may either aid viral entry or inhibit it. Unlike most other pathogens, viruses generally do not possess glycosylation machinery and instead use the host cell machinery to replicate.
The glycans present on viral proteins are essential to enabling access to host proteases and antibodies. Viruses use the carbohydrate-binding receptors as a means of accessing host cells and their glycosylation machinery as a way of hiding potential immunogenic epitopes.
Low-affinity antibodies that target certain viral glycosylated proteins have also been shown to contribute to infection, and the glycosylation profile of the SARS-CoV-2 spike protein has recently been described in this context.
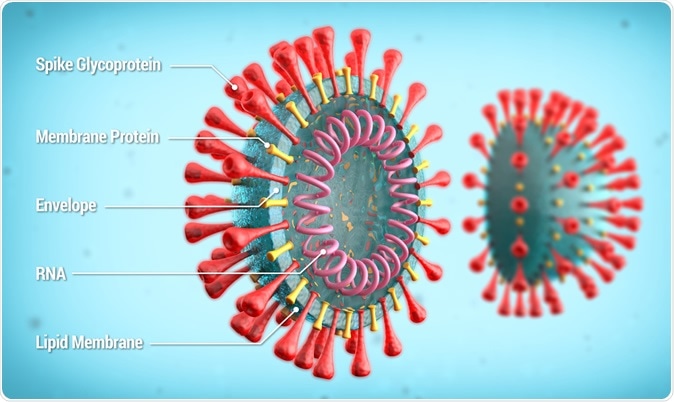
Labeled diagram of SARS-CoV-2 showing spike glycoprotein, membrane protein, envelope, RNA. Credit: lmt3d / Shutterstock
Research looking at human embryonic kidney cells (HEK293) found that the N-glycosylation profile of this protein included high mannose glycans and complex-type oligosaccharides at various glycosylation sites.
Improving understanding of the carbohydrate-mediated binding of SARS-CoV-2
To better understand the carbohydrate-binding receptors that may enable viral entry and contribute to immune-modulatory responses, the researchers performed solid-phase immune assays using HEK293 cells to explore interactions between the spike protein and 12 host lectin receptors involved in inducing and modulating immune responses.
The team found that the SARS-CoV-2 spike protein specifically bound to certain lectin receptors that are expressed on myeloid cells such as dendritic cells and macrophages. The receptors were Dendritic Cell-Specific Intercellular adhesion molecule-3-Grabbing Non-integrin (DC-SIGN), Macrophage galactose binding lectin (MGL), sialic acid-binding immunoglobulin-type lectins (Siglec)- 9 and Siglec-10.
To also better understand how the lung microbiota might promote or modulate viral infection, the team explored interactions between the spike protein and a range of Streptococcus pneumoniae polysaccharides and other microbial glycoconjugates.
The researchers report that the spike protein bound specifically to two S. pneumoniae polysaccharide serotypes. It also bound to a glycoconjugate on Pseudomonas aeruginosa, a leading cause of acute hospital-acquired infections and pneumonia.
What are the implications of the study?
The researchers say that, interestingly, they found that specific rhamnosylated epitopes in lung microbiota were a discriminating factor for spike protein binding, potentially providing a link between the presence of certain lung microbiota, SARS-CoV-2 infection and the severity of the disease.
“These observations could trigger the design of new therapeutic approaches for the bacterial co-infections in COVID-19 patients,” suggests the team.
“In conclusion, we revealed novel ACE2-independent carbohydrate-mediated interactions with immune-modulating lectins expressed on myeloid cells, as well as host lung microbiota glycoconjugates,” write the researchers.
They suggest that these new molecular pathways they have identified may contribute to and drive viral infection severity and, subsequently, an exacerbated, uncontrolled immune response and inflammation.
“These results may have implications to control and understand the bacterial co-infections, to have a better understanding of the disease severity and to add risk factors in COVID-19 patients,” say Chiodo and team. “Together, these data aim at adding different carbohydrate-mediated interactions in the complex and holistic picture of the SARS-CoV-2 infection and its implications.”