Public awareness matters amid the coronavirus disease (COVID-19) pandemic; however, a new study shows that more than 92 percent of the Australian population cannot differentiate between a bacterial and viral infection.
A survey was carried out by the Commonwealth Scientific and Industrial Research Organization (CSIRO) in March, as part of the OUTBREAK project, which is a multi-agency mission that aims to prevent outbreaks of superbugs or antibiotic-resistant bacterial infections.
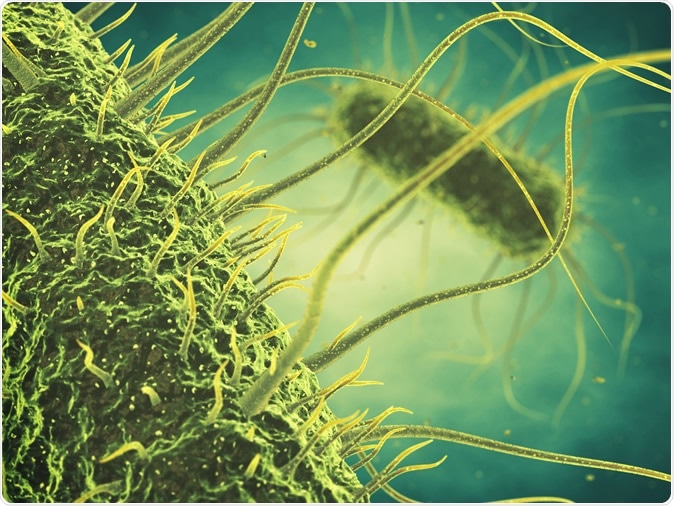
Salmonella bacteria 3d illustration. Image Credit: nobeastsofierce / Shutterstock
The survey
The survey, covering more than 2,200 people, revealed a worrying fact that there is still limited knowledge about pathogens and the use of antibiotics. The team found that about 13 percent of Australians believe that the COVID-19 can be treated with antibiotics, even though it is a viral infection.
Further, it was unveiled that as many as 92 percent of Australians did not know the difference between viral and bacterial infections, while 19 percent thought antibiotics are required for common colds. Another 14 percent have consumed antibiotics when traveling to other countries, thinking they will be protected from infections.
More than a third of the respondents believe antibiotics can cure a sore throat or flu, while about 15 percent assumed antibiotics could be effective against diarrhea or chickenpox.
When asked about the difference between a bacterial and a virus, 64 percent of the respondents said they are unsure.
Viruses and Bacteria
A viral disease (or viral infection, or infectious disease) occurs when pathogenic viruses invade an organism's body, and infectious virus particles (virions) attach to and enter susceptible cells.
Bacteria are single-celled microorganisms that thrive in many different types of environments. Though most bacteria are harmless or often beneficial, some are pathogenic, with the number of species estimated as fewer than a hundred that are seen to cause infectious diseases in humans. If bacteria form a parasitic association with other organisms, they are classed as pathogens.
The OUTBREAK project
The OUTBREAK project, which was established in 2019, aims to use artificial intelligence to predict superbug outbreaks. The team also wants to share information about antibiotic-resistant pathogens and how they can negatively impact populations.
“OUTBREAK uses a One Health approach, which means that, as well as people, we will look at how animals, plants and the environment contribute to antimicrobial resistance. This will help us to intervene in ways that will have the greatest positive impact on our health and economy,” Prof. Branwen Morgan from UTS and OUTBREAK CEO, said.
“Drug-resistant bacteria can infect anyone regardless of age, gender, or location. To fight them, we need to fully understand which ones are a threat to our health and how they are spreading into and within Australia,” he added.
The project is led by the University of Technology Sydney, alongside other organizations such as CSIRO, the University of South Australia, Sax Institute, NSW Department of Primary Industries, the University of South Australia, and Oracle, among others.
Superbugs on the rise
Due to misinformation and lack of knowledge, antibiotic drug resistance is a significant health problem worldwide. The survey states that superbugs or drug-resistant bacteria could cause up to 10 million deaths per year by 2050. So far, more than 700,000 people have already died across the globe in the past year due to the overuse of antibiotics.
“The misuse and overuse of antibiotics is a huge problem because it’s fueling the rise of drug-resistant ‘superbugs,’ which causes life-threatening infections but are immune to routine antibiotics. When we run out of effective antibiotics, we’ll be back in the ‘medical dark ages’ of the pre-1940s, where a scratch or simple infection killed, so the public must be educated on this issue,” Paul De Barro, CSIRO biosecurity research director, said.
Antibiotics may lose their effectiveness if they are misused and overused. They are hard to replace; hence, they need to be used properly and for the right reasons.
Health teachings and education can help in informing patients on how antibiotics work and how they should be taken. This way, overuse will be reduced, reducing rates of antibiotic-resistant pathogens.
Knowing the difference between viruses and bacteria is crucial to know when an antibiotic can treat a disease. Consulting with a doctor for illnesses should be done to prevent self-medicating with medicines that may not be needed.