A pre-print version of the study can be accessed on the bioRxiv* server, while the manuscript undergoes peer review.
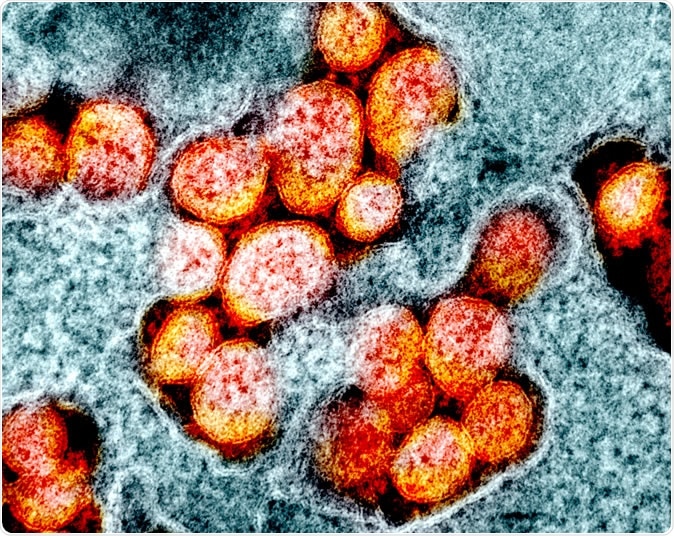
Novel Coronavirus SARS-CoV-2 Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The “guardian of healthspan”
As a regulator of cellular redox balance, Nrf2 is often referred to as the “guardian of healthspan,” since it protects against the oxidative stress that can lead to various metabolic and degenerative diseases.
Importantly, the levels of this transcription factor decrease with age. The loss of Nrf2 allows oxidative stress to go unchecked and drives the frailty associated with aging due to disrupted proteostasis, altered genomic stability, increased susceptibility to infection, and cell death.
“It is this age-related frailty that often defines the most vulnerable population in situations such as the one we currently face with the coronavirus pandemic,” writes Joe McCord (Pathways Bioscience, Aurora, USA) and colleagues.
Investigating the effects of Nrf2 activation in human cells
For a virus to be able to replicate, it needs to sustain oxidative stress at a higher level than usual, but not so high as to destroy host cells. Viruses have “learned” to manipulate the Nrf2 pathway in ways that confer survival and enable them to take control from host cells.
Recently, McCord and the team described a potent Nrf2 activator called PB125, which they have now investigated the effects of in human liver-derived HepG2 cells and pulmonary artery endothelial cells.
The team wanted to investigate the changes in gene expression as a result of Nrf2 activation that may be involved in antiviral activity overall, as well as those specifically involved in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the associated COVID-19.
SARS-CoV-2 has a unique way of entering host cells
Unlike many families of viruses that share common modes of host cell entry such as intercellular adhesion molecule 1 (ICAM-1) and low-density lipoprotein (LDL) receptor, SARS-CoV-2 seems to be limited to one specific mode of entry.
This unique entry mode may represent the virus’s most significant weakness since pharmaceutical agents could potentially target it and block host cell entry.
The binding of the spike protein that enables SARS-CoV-2 to enter target cells is dependent on the host cell receptor angiotensin-converting enzyme (ACE2). It also requires priming by a transmembrane enzyme encoded by the gene TMPRSS2, which involves cleavage of the spike protein to allow fusion to the host cell membrane.
Now, McCord and colleagues have demonstrated that PB125 downregulated the expression of ACE2 by 3.5 times, TMPRSS2 by 2.8 times, and upregulated a potent inhibitor of TMPRSS2 called PAI-1 by 17.8 times.
The researchers say the findings “strongly suggest that PB125 treatment might diminish the ability of SARS-CoV-2 to bind to a host cell and to obtain spike protein activation as a result of less ACE2 and TMPRSS2 on the cell surface, and as a result of a 17.8-fold increase in plasma PAI-1, which would inhibit the remaining TMPRSS2.”
How is the cytokine storm involved?
A cytokine storm is a type of systemic inflammation that can be induced by infection when large numbers of white blood cells become activated and produce inflammatory cytokines that then activate more white blood cells.
The inflammation that occurs in COVID-19 is associated with such an increase in inflammatory cytokines, interleukins, tumor necrosis factor-α (TNF), and granulocyte colony-stimulating factor (GCSF).
Of forty-one COVID-19 patients hospitalized in Wuhan, China, all had high levels of interleukin 1B and the chemokines IP10/CXCL10 and MCP1/CCL2. Sixteen of them who were then sent to ICU had even higher levels of these cytokines, and the extent of the cytokine storm strongly predicted prognosis and mortality.
The researchers say their study found that the genes encoding these cytokines were significantly down-regulated after treatment with PB125 treatment.
“We propose that it is a robust oxidative stress-induced activation of Nrf2 in young, healthy individuals that follows the gathering storm and rescues host tissues from irretrievable self-inflicted damage,” writes the team. “In older individuals, or in the presence of comorbidities that may involve chronic inflammation, the Nrf2-activation response may be insufficient to break the self-perpetuating cycle of events.”
What are the implications of the findings?
The team suggests that among elderly or otherwise compromised patients, activating more of the limited amount of Nrf2 they have left might stop the cytokine storm and help patients enter the recovery and repair phase of the inflammation response.
“This activation boost to suboptimal levels of Nrf2 can be provided by several pharmacological agents, and as well or better by a number of phytochemical activators, as we show here with PB125,” advise McCord and team.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources