Many lives have been lost to the severe pneumonic disease COVID-19 caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), during the ongoing pandemic. The reason for the critical lung injury that results in a fatal outcome in a significant minority of patients has been supposed to be the dramatic oversecretion of pro-inflammatory cytokines and chemokines triggered by the virus.
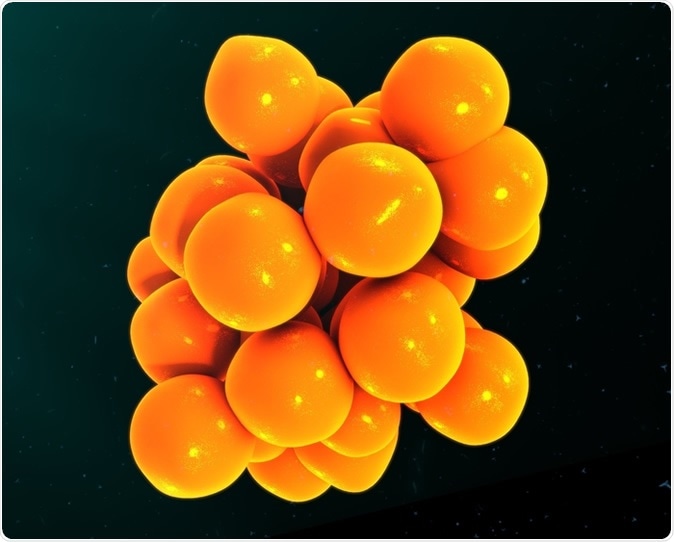
Cytokines 3d illustration. Image Credit: sciencepics / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Finding the Truth About the Cytokine Storm
The current study by researchers at Stanford University and published on the preprint server medRxiv* aims to uncover the true magnitude of the elevation in inflammatory cytokines in patients with severe COVID-19, to determine if this is truly a unique phenomenon or simply one that results in many similar conditions, such as acute respiratory distress syndrome (ARDS) or patients who are critically ill with sepsis.
All three states are known to be associated with high levels of inflammation. However, the trials carried out on the therapeutic use of immune modulators like anti-ILb, activated protein C and steroids on large numbers of COVID-19 patients have not displayed notable success. In fact, one recent report shows that IL-6 levels in severely ill patients with COVID-19 are actually lower than those from earlier series of patients with ARDS, at 10-40 pg/mL vs. 100-2000 pg/mL.
In the current study, there were nine patients with severe COVID-19, with mechanical ventilation being necessary for 6 of them. Of the 6, 5 had moderate to severe ARDS, and all had to be on the ventilator for a week or more.
Granted that the measurement of cytokines across different platforms can differ, the researchers measured the plasma levels of 76 cytokines in a group of patients in hospital with COVID-19, as a prospective study. Among these, six are the inflammatory cytokines found in cytokine storms. These are IL-1b, IL-1RA, IL-6, IL-8, IL-18, and TNFα.
The measured levels were then compared to those in blood specimens from patients with ARDS and sepsis, from Stanford ICU Biobank of biospecimens collected before the current pandemic broke out.
Are cytokines markedly higher in severe COVID-19?
The researchers found no marked differences between the levels of these six inflammatory biomarkers between patients with severe or moderate COVID-19, ARDS, or sepsis. Severely ill COVID-19 patients showed a nonsignificant trend towards higher IL-1RA and IL-6 levels compared to those with moderate illness, as expected, and also a trend towards higher IL-18 compared to those with other critical conditions.
When the full range of 76 cytokines is considered, there was no significant difference between the three groups of patients. Small individually significant differences may be noted in the case of a few cytokines, but no outstandingly distinct elevations for any cytokine.
In other words, say the researchers, “these data suggest that a “cytokine storm” in COVID-19 that is distinct from other critical illness (e.g., sepsis and ARDS) is unlikely.” Instead, they suggest, the elevated cytokines are merely what should be expected in any critically ill patients.
A very small sample using the 6 IL-6 samples collected by the hospital laboratory independently showed its levels to be <6-31 pg/mL. While this is too small to come to a reliable conclusion, it does show that this cytokine is no higher in patients with severe COVID-19 than any other patient with serious illness.
Cytokine Elevation Reflects High Viral Load
Rather, therefore, than labeling the cytokine elevation as the major cause of the increased mortality and morbidity in severe COVID-19, the researchers agree that it is a response to a high virus burden rather than an inappropriately high host immune response which should be modulated.
The small sample size makes it difficult to detect minor differences in the cytokine profile. Additionally, longitudinal follow-up was not performed, providing only a snapshot at the time of entry into the study. The unit of measurement is also different in the current study, which hinders direct comparison without unit conversion.
The conclusions hold good, despite these limitations, that the cytokine elevation in this condition is no different from that seen in other critical illnesses. The right response should not be, therefore, broad application of immunosuppressive therapies, as has been tried for decades in both sepsis and ARDS patients.
The only outcomes of such trials have been potential harm to some patients, at least, to counterbalance the possibility of improvement in a few. The researchers comment, “Indeed, given the duration of mechanical ventilation and attendant high rates of nosocomial infection in severe COVID-19 patients, these therapies have the potential for harm.”
Thus, more study is required to understand in the detailed immune response to COVID-19 and to identify those patients at least risk of harm and maximum potential for improvement with immunomodulatory drugs.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources