As the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) continues to ravage the world, scientists are frantically searching for a vaccine or new drug that will effectively counter the lethal effects of the virus that leads to COVID-19 disease.
Now, new research from the University of Texas Medical Branch at Galveston and published on the preprint server bioRxiv* shows SARS-CoV-2 replication and respiratory disease can be produced in African green monkeys using a much lower and more natural dose of SARS-CoV-2 than has been employed in other non-human primates studies.
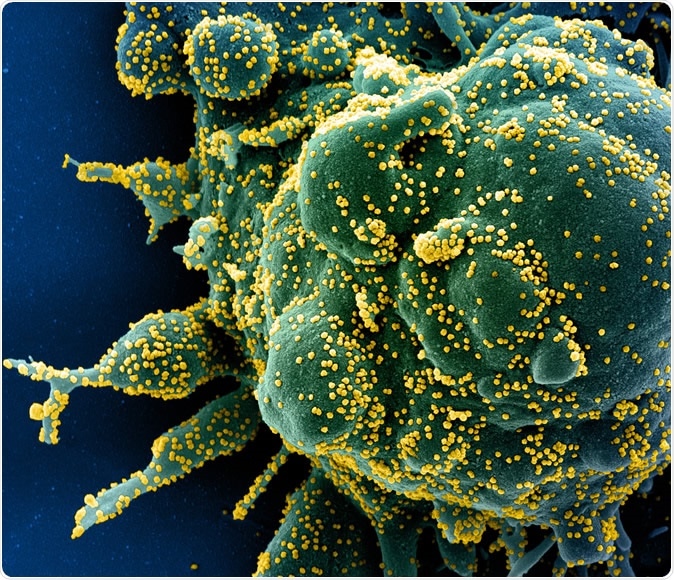
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of an apoptotic cell (green) heavily infected with SARS-COV-2 virus particles (yellow), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Why are animal models useful?
An effective vaccine is the only way to ensure COVID-19 is totally eradicated. A detailed understanding of how the virus achieves its damaging effects, and of the illness itself, are fundamental to building a vaccine or drug. Such vaccines need to be tested in animals during preclinical studies to reveal any potential adverse severe effects and find an effective dosage.
However, SARS-CoV viruses show a propensity to unwanted immune activation following immunization with candidate vaccines of various types. These include inactivated whole virus, recombinant DNA subunit, virus-like particles, and live attenuated virus based on vector use.
The same type of hypersensitivity reaction to the virus is also seen after the induction of infection in experimental animals. The close similarity between SARS-CoV and SARS-CoV-2 mandates careful evaluation of any candidate vaccine before it enters human trials.
This, in turn, means that a suitable animal model is essential to rule out such immune complications before such vaccines are commercially released. Such models will also help uncover the mechanics of disease spread and virus-immune interactions.
Features of an ideal animal model
Many animal models allow SARS-CoV-2 replication and also develop non-fatal illness to varying degrees after exposure to the virus through their respiratory tracts. These include mice, hamsters, ferrets, and non-human primates (NHPs).
Each of these models is useful in one or more ways to study the virus and the illness. However, NHPs are more reliable when it comes to comparing the host responses to infection in humans because of their genetic similarity. This also underlies the development of reagents to study the immune response.
It was in the recent weeks that the earliest assessment of the utility of Rhesus and cynomolgus macaques was reported. The difference in clinical features in these two NHPs indicates a greater suitability of some species compared to others, to serve as human models of CoV infection.
African Green Monkeys as a SARS-CoV-2 model
For the earlier SARS-CoV, African green monkeys (AGM) supported viral replication most efficiently, compared to Rhesus and Cynomolgus macaques, and only the first species showed significant replication in the lower respiratory tract after inoculation with SARS-CoV. The autopsy findings in these animals also showed features of disease similar to that in humans. They also have the same viral receptor, ACE2.
These features brought them to the attention of researchers in the current study. The animals were inoculated with a low-passage isolate of SARS-CoV-2 to test their potential as a model for this infection. The strain used was from the first clinical case in Italy, and the first virus from clade V to be used to induce experimental infection in NHPs.
The AGMs are shown to replicate several aspects of disease in humans, including high levels of viral replication and pneumonic lesions. Thus, this is a suitable model to study the process of disease in humans as well as to screen potential vaccines and therapeutics.
The researchers found that at 0, 2, 3, 4, 5, 7, 9, 12, 15, and 21 days following inoculation with the Italian isolate by both intratracheal and intranasal instillation, no clinical signs of disease were found. Imaging was also inconclusive. Three of the animals were sacrificed on day 5 but showed some signs of pneumonia with hyperemia.
Nasal secretions showed viral RNA and infectious viral particles in three animals, but the rectal swab in one animal only showed infectious viruses, while another two showed viral RNA. All animals showed the presence of both in bronchoalveolar lavage fluid, but not in plasma.
Inflammatory markers were increased, including IL-8, IL-10, IL-12, and IL-6. The latter is an activator of inflammatory pathways and predicts respiratory failure in humans with COVID-19. Fibrinogen levels were high, as is in keeping with the known role of IL-6 in fibrinogen synthesis as an acute phase change, and the presence of bleeds in the lungs.
AGM Model Helps Clarify Some Diagnostic Points
Overall, the AGMs failed to show signs of overwhelming illness, even while there were changes in the lungs and the blood, showing that the animals were suffering infection with systemic responses. The failure of chest X-rays to show changes in keeping with the lung lesions has implications for the reliability of this imaging technique as a screening method for humans as well. The use of CT scans or plethysmography could be a more dependable way to visualize lung lesions in animal models.
A second exciting sidelight is the presence of gut lesions in infected AGMs, as has been noted in humans as well. This reflects the expression of the ACE2 receptor in the gut epithelium as well. Despite the presence of such injury, there were no overt gut-related symptoms, except for a loss of appetite in most animals around the third day from infection.
The study shows that “infection of AGMs with SARS-CoV-2 results in the release of inflammatory mediators with similar immune signatures as human cases.” The changes in laboratory parameters and markers of inflammation underline the utility of this model in the study of the host response to COVID-19.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources