The current pandemic of COVID-19, which started in 2020, has now spread to almost all the countries of the world, with over 4.88 million cases and more than 322,000 lives lost. Emerging in Wuhan, China, it rapidly spread to Europe. Italy quickly became an epicenter, with over 226,000 cases and 32,000 deaths.
Overall, about 80% of COVID-19 patients show mild symptoms or none. About 14% develop severe pneumonia, requiring hospitalization, while the remaining become critically ill, requiring intensive care unit (ICU) admission.
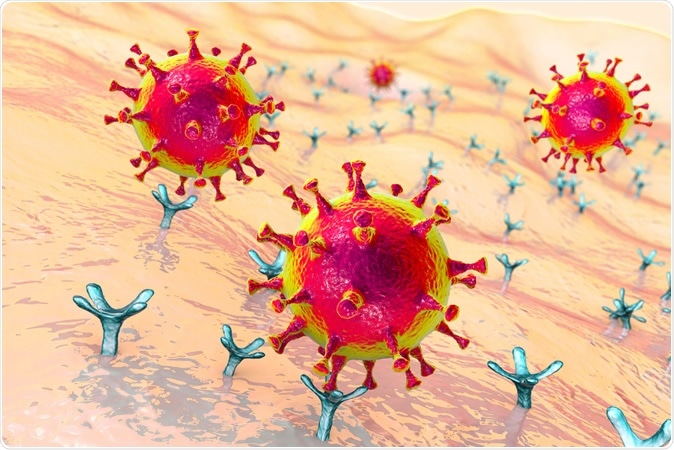
SARS-CoV-2 viruses binding to ACE-2 receptors on a human cell, the initial stage of COVID-19 infection, conceptual 3D illustration Credit: Kateryna Kon / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The Pro-Inflammatory/Anti-Inflammatory Imbalance
For many researchers, this was thought to be the result of a cytokine storm due to the overactivation of immune cells, mediated by the key cytokine IL-6. As a result, the anti-IL-6 monoclonal antibody tocilizumab was approved and used to treat severe COVID-19 pneumonia.
However, the stocks of this drug in Italy rapidly vanished as the demand mounted. This led to the use of another IL-6 inhibitor called Sarilumab, which is also an FDA-approved drug for rheumatoid arthritis (RA).
Sarilumab In Severe COVID-19
The current study was aimed at exploring the effects of off-label use of Sarilumab in these patients with severe pneumonia caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The chosen outcomes were to evaluate the effect of Sarilumab in these cases, with respect to improvement in lung function and prevention of ICU admission, safety, and the hypothetical biological and clinical measures that indicate improvement or transfer out from ICU following Sarilumab.
The study covered 53 hospitalized patients with severe pneumonia related to SARS-CoV-2, between March 23 and April 4, 2020. Each patient was followed up for 14 days or more. Each patient received 400 mg of Sarilumab with a second dose if the clinical condition worsened or failed to improve. Repeat doses were needed in
Patients hospitalized for COVID-19 also received lopinavir/ritonavir combination or darunavir/ritonavir combination (70% and 25% respectively), hydroxychloroquine (94%), azithromycin (55%), and prophylactic heparin (75%). Patients were tested for lung function, oxygen demand, and blood testing, including plasma IL-6 levels.
Almost 90% of patients were male, and the median age was 66 years, 62% to 64 % were either overweight or had one or more coexisting medical conditions. A third of them received only one dose of Sarilumab.
Of the total 53 patients, 74% were treated in the medical wards and 26% in the ICU. Two-thirds of the first group had a single dose, while about 93% of those in the ICU required two doses.
The Effects of Sarilumab
Among almost 40 patients in the medical wards, 18% required ICU care. Of these, 57% were shifted back to the ward with improvement in 5-8 days. The improvement among the 40 patients occurred after 24 hours from the infusion of Sarilumab in 46% and 64% at three days.
At the last contact, 90% showed a positive response. Oxygen was not required for 86% of them, and 71% were discharged to home.
Of the 14 patients in the ICU, two-thirds were discharged to the medical ward within 12 days of Sarilumab administration. 90% of this group had improved to not needing supplementary oxygen at the last contact. Of the remaining five patients in the ICU, none had died within this period.
The overall mortality following the administration of the drug was 6%.
Predicting the Efficacy and Need for ICU Care
Patients who recovered were likely to be younger, with less lung damage, a lower ratio of neutrophils to lymphocytes, and with lower initial IL-6 levels. A combination of age, better initial respiratory parameters (pre-treatment PaO/FiO2), and lower initial IL-6 levels predicted the highest odds that Sarilumab would be effective, producing an early response and lower chances of requiring ICU care.
The researchers observe that a randomized controlled trial will be required to reveal the possibility of controlling the inflammatory process better in aggressive cases by a higher dosage of the drug, or a more significant number of infusions.
On the other hand, this type of nomogram using multiple variables can predict the need for ICU transfer in up to 80% of patients with severe pneumonia. An interesting sidelight that arose from the study is the observation that the earlier the start of therapy with Sarilumab, the sooner was the positive result, that is, clinical improvement. Thus, the study points to the existence of a window of opportunity to change the clinical course of the disease.
The study has several limitations. It used an open-label approach, employed no controls, and had a small number of patients with critical disease, besides using other treatments simultaneously with Sarilumab, of unknown effectiveness. The follow-up may also be too short to assess the long-term efficacy and record any serious adverse effects of Sarilumab therapy.
The researchers conclude: “IL-6R inhibition is a successful treatment strategy for severe SARS-CoV-2 pneumonia and Sarilumab is a valid and safe alternative in the therapeutic armamentarium of this disease without defined standardized treatment algorithms. (sic)”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Gremese, E., et al. (2020). Sarilumab use in severe SARS-CoV-2 pneumonia. medRxiv preprint doi: https://doi.org/10.1101/2020.05.14.20094144. https://www.medrxiv.org/content/10.1101/2020.05.14.20094144v1
- Peer reviewed and published scientific report.
Gremese, Elisa, Antonella Cingolani, Silvia Laura Bosello, Stefano Alivernini, Barbara Tolusso, Simone Perniola, Francesco Landi, et al. 2020. “Sarilumab Use in Severe SARS-CoV-2 Pneumonia.” EClinicalMedicine 27 (October): 100553. https://doi.org/10.1016/j.eclinm.2020.100553. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(20)30297-2/fulltext.