Researchers at Wayne State University and Henry Ford Health System in Michigan have conducted a study indicating that the corticosteroid methylprednisolone could improve outcomes among patients with severe coronavirus disease 2019 (COVID-19).
However, although this may appear to support the use of corticosteroids to treat COVID-19, the team warns that not all drugs in this class are expected to improve outcomes since other types did not have similar effects.
“For instance, methylprednisolone and prednisolone were predicted to be effective in reverting many of the changes triggered by COVID-19, while other closely-related steroids such as prednisone or dexamethasone were not,” write Sorin Draghici (Department of Computer Science, Wayne State University) and colleagues.
The team says the findings have important implications for any pandemic in the future, irrespective of the virus involved.
A pre-print version of the article can be accessed on the server medRxiv*, while the article undergoes peer review.
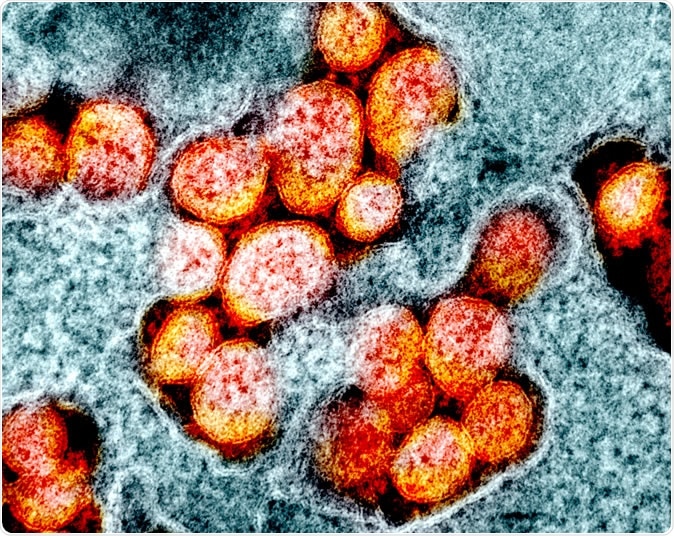
Novel Coronavirus SARS-CoV-2 Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Current efforts to manage COVID-19
Currently, efforts to manage COVID-19 include early diagnosis, antiviral medications, modulation of the immune system, and vaccine research and development.
However, Draghici and colleagues say one crucial aspect that should be included is the identification and treatment of patients developing a hyperinflammatory response called the cytokine storm - a cascade of inflammatory reactions that can be critical and fatal.
“Treatment of this hyper-inflammation in these patients using existing, approved therapies with proven safety profiles could address the immediate need to reduce the rising mortality,” writes the team.
What were the aims of this study?
This study aimed to, first, understand the immune response to COVID-19 in lung epithelial cells and, second, to find drugs that would reduce damaging and potentially fatal immune system overreactions.
The researchers used transcriptomic data to compare mock infection of an A549 cell line (adenocarcinoma human alveolar basal epithelial cells) and primary human bronchial epithelial (NBHE) cells with infection by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), seasonal influenza A and human respiratory syncytial virus.
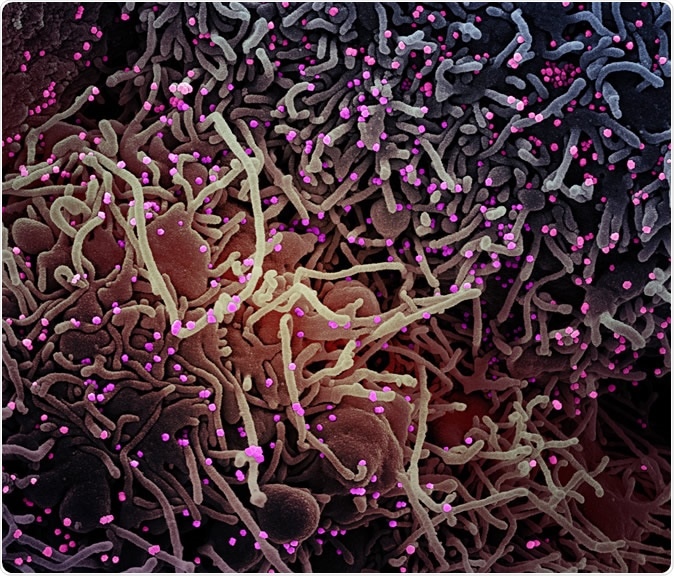
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of a VERO E6 cell (purple) exhibiting elongated cell projections and signs of apoptosis, after infection with SARS-COV-2 virus particles (pink), which were isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
They also compared changes in gene expression, pathways, and mechanisms between lung tissue infected with COVID-19 and healthy lung tissue.
Identifying FDA-approved drugs
Once the team had identified the key pathways that seemed to be linked to hyperinflammation, they identified, in silico, FDA-approved drugs that exerted activity on various components of inflammation and could, therefore, potentially be repurposed to help manage patients with severe COVID-19.
“An important finding is that drugs in the same class will not achieve similar effects,” writes the team.
Methylprednisolone was identified as the drug most likely to work; it targeted 27 genes that were differentially expressed in COVID-19-infected tissues versus healthy lung tissues.
Prednisolone was also predicted to be effective at reverting many of the changes caused by COVID-19.
Not all corticosteroids tested were effective
However, the closely-related corticosteroids, namely prednisone, dexamethasone, and hydrocortisone, were not effective at reverting the changes. Prednisone only targeted three differentially expressed genes in COVID-19-infected versus healthy lung tissue, and of those, it only reverted one. Prednisone also targeted two genes in the NHBE cells, but it was not effective at reverting either of them.
Neither dexamethasone nor hydrocortisone seemed to be effective in the COVID-19 tissue, although hydrocortisone seemed to have a marginal effect on NHBE cells.
Clinical validation of the findings
To validate their findings, the team conducted an independent pre-and post-treatment study of methylprednisolone, including 213 patients with severe-to-moderate COVID-19 who were hospitalized at a health center in Michigan.
The composite primary endpoint, which was the need for ICU, the need for mechanical ventilation and death, occurred at a significantly lower rate among the post-treatment group (34.9%), compared with the pre-treatment group (54.3%). The median length of hospital stay was also significantly reduced in the post-treatment group (5 days), compared with the pre-treatment group (8 days).
The findings are consistent with those of recent studies
The authors refer to two recent studies, one reporting that it does not support the use of corticosteroids in the treatment of COVID-19 and one reporting that methylprednisolone was effective at decreasing the risk of mortality among COVID-19 patients with acute respiratory distress syndrome.
“Both reports are entirely consistent with our findings,” say Draghici and colleagues… “Corticosteroids, in general, are NOT expected to help as a class of drugs. However, methylprednisolone and prednisolone are targeting a large number of the genes affected by COVID-19 and are expected to work significantly better than other corticosteroids.”
The researchers say their findings have important implications for any pandemic in the future, irrespective of the virus involved.
“A SARS-CoV2-specific vaccine or a SARS-CoV2-specific antiviral will reduce the impact of this particular virus in future seasons,” writes the team. “However, better understanding the acute reaction of the immune systems and having more tools to mitigate or avoid a cytokine storm will be important for any future pandemic regardless of the virus.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Source:
Journal references:
- Preliminary scientific report.
Draghici S, et al. COVID-19: disease pathways and gene expression changes predict methylprednisolone can improve outcome in severe cases. medRxiv 2020. doi: https://doi.org/10.1101/2020.05.06.20076687
- Peer reviewed and published scientific report.
Draghici, Sorin, Tuan-Minh Nguyen, Larry A Sonna, Cordelia Ziraldo, Radu Vanciu, Raef Fadel, Austin Morrison, et al. 2021. “COVID-19: Disease Pathways and Gene Expression Changes Predict Methylprednisolone Can Improve Outcome in Severe Cases.” Edited by Janet Kelso. Bioinformatics, March. https://doi.org/10.1093/bioinformatics/btab163. https://academic.oup.com/bioinformatics/article/37/17/2691/6164952.