Ever since the beginning of the international spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that causes COVID-19 disease, researchers have been trying to identify the risk factors that increase the chances of infection. Now, a new study published on the preprint server medRxiv* in May 2020 discusses various potential factors and reports the observed associations.
Earlier studies show that both symptomatic and asymptomatic individuals can spread COVID-19 to uninfected people. The virus is transmitted mainly through respiratory droplets, or through contaminated surfaces and objects. The most common initial symptoms include fever, dry cough, and tiredness, but atypical manifestations are being seen as well.
Most population-based research on the incidence of COVID-19 shows that advancing age and the presence of underlying conditions like diabetes, hypertension, and cardiovascular disease can lead to more severe illness. Other risk factors that have been discussed include gender, Bacillus Calmette-Guerin (BCG) vaccination, smoking, and malaria prevalence
The reason for the increased risk in older individuals could be age-dependent senescence of the lymphocytes, the immune cells that play a significant role in clearing the virus from the body.
The BCG vaccination is thought to stimulate nonspecific cellular immunity, while malaria may induce immune tolerance, thus dampening the hypothesized cytokine storm produced by an overactive immune response to the virus.
It is essential to identify the risk factors for COVID-19 since this could help triage infected patients who need more intensive care. The current study is aimed at presenting a clinical picture of the split-up of the case fatality rate (CFR) in the 50 countries that have been affected the most. This has been used to set up a predictive model of the infection and case fatality rate of COVID-19.
The researchers from Brunei, China, Malaysia and Singapore recovered demographic and epidemiologic data from the World Bank and John Hopkins University COVID-19 websites. They evaluated the number of confirmed cases and deaths. They also extracted the indicators of the factors that affect the risk of this condition. In particular, they looked at the proportion of people aged 65 and above in each country, the proportion of males, the prevalence of diabetes, and smoking, the health expenditure, the number of hospital beds and the number of nurses/midwives combined.
The study used information on just over 2 million cases and 137,000 deaths due to COVID-19, which was about 93% of the cases and deaths globally as of April 16, 2020. The percentage of confirmed COVID-19 cases per country was calculated by dividing the number of confirmed COVID-19 cases by the total population for each country. The CFR was calculated by dividing the number of deaths related to COVID-19 by the number of confirmed cases.
The USA was found to have the highest number of both confirmed cases and deaths, with a percentage of 0.20% and a CFR of 4.85%. On the other hand, Luxembourg, which then stood at the 47th place, has the highest percentage of cases at 0.55%, but a low CFR of 2.05%. In other words, a high case number doesn’t always mean a high CFR.
The study thus shows differences in the number of cases, transmission, and severity of disease between countries that do not always correlate with the ranking system. This underlines the need to understand the risk factors that can influence the increase in the mortality rate of this disease.
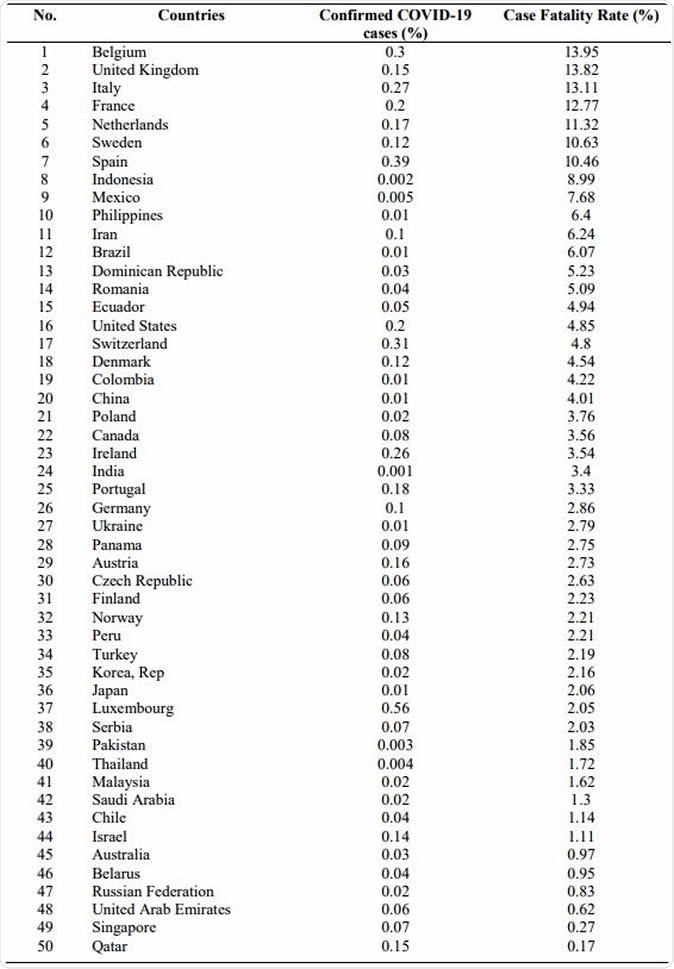
Percentage of confirmed CFR and COVID-19 cases (In sequence of the highest to lowest CFR%)
Age and COVID-19 Risk
The number of people aged 65 and above is significantly linked to the CFR, which goes up by 4.7 units for every 1-unit increase in the proportion of people at or above this age. When this proportion crosses 0.15, there is a spike in the CFR as well.
Earlier studies have shown this trend since, in Seattle, the US reported over 60% of deaths in this age group. Other studies confirm a CFR of 4.5% for those above 60 but 1.4% for those below. In people above 80, the CFR may be above 13%.
The average age of patients who died of COVID-19 was 68, while that of patients who recovered was 51 years.
Immune system decline may be among the chief contributors to this trend, since both T and B cell function decrease, while type 2 cytokines are overproduced. This is thought to stimulate viral replication and prolong the period of pro-inflammatory responses, causing poor health.
Secondly, older people may have more underlying medical conditions, which are known to increase the risk of severe illness following COVID-19 infection.
Diabetes and COVID-19 Risk
The prevalence of diabetes is inversely linked to the CFR, which is lower by 0.97 units in the countries with the highest prevalence when compared to those with the lowest. This is in contradiction to many other studies that have shown that many severely ill patients with COVID-19 are those who have diabetes or hypertension.
When both these factors are incorporated into the analysis, no significant association is found, however.
Male Sex and COVID-19 Risk
The study failed to show any association between male sex and the COVID-19 CFR. However, other researchers have shown that this illness preponderantly affects males over females. The reasons could be diverse, ranging from the existence of more underlying health factors compared to the female segment of the population, or the male tendency towards more risky behaviors that can impact health, such as smoking and drinking.
Genetic factors, and inherent differences in the way the immune system responds to infection, could also come into play here.
Other Risk Factors
Smoking was not found to have a significant association with the occurrence of COVID-19. Still, since other factors were not examined, the researchers caution against assuming “that there is no correlation between other co-morbidities and COVID-19 CFR since not all factors were considered in this study, such as hypertension and cardiovascular diseases.”
Many other studies have shown a high proportion of hypertension in patients who died of COVID-19. The reasons may be due to vascular aging, reduced renal function, and interactions between different medications used for various conditions, including COVID-19.
Healthcare Expenditure and CFR
The current study did not confirm a link between a higher CFR and a lower level of healthcare infrastructure or expenditure. This could indicate the degree to which preparedness plans were set in motion to flatten the curve of the outbreak in different countries. These include ensuring the availability of medical supplies, quarantine centers, healthcare personnel, and the designing of appropriate strategies to minimize viral spread.
On the other hand, high death and infection rates were reported in Italy, including many among healthcare workers because personal protective equipment (PPE) was lacking. The projected lack of ventilators in the US is also a worrying concern.
Having the right number of healthcare workers is also vital in controlling the epidemic since this not only prevents shortages but also assures the right amount of rest and support for those under stress.
Limitations and Conclusion
The study is poorly designed in many respects. Firstly, it does not account for a number of factors like malaria prevalence. The data for different indicators comes from different years. Even for a single indicator, the data did not come from a single year.
The researchers say, “Potential risk factors need a lot more research in order to understand the risks for the worst forms of COVID-19 and what we ought to learn to best protect the most vulnerable people.”
Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.