The current pandemic of COVID-19 has caused many millions of people to become sick, and hundreds of thousands have been left dead. However, without a clear understanding of how its fatal effects are brought about, there is a lack of effective management strategies. A new study published on the preprint server medRxiv* in May 2020 reports the discovery of a predictive pattern of cytokines in COVID-19 infection that could guide clinical management if validated.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Uncontrolled Inflammation and COVID-19
Many scientists think that the high mortality rate of the COVID-19 outbreak is due to a combination of direct viral injury and uncontrolled release of inflammatory cytokines that worsen tissue damage. This type of cytokine storm is not unique to COVID-19, however. In fact, it is similar to the cytokine release syndrome (CRS) seen with CAR-T cell therapy in cancer patients.
One cytokine believed to be involved in CRS is IL-6, based on the use of tocilizumab has widely used to treat such patients. This has been extended recently to COVID-19 patients as well, but with qualified success only.
Another cytokine that is higher in CRS is TNF-alpha, which amplifies inflammatory response pathways. Drugs that inhibit TNF-alpha are at present being used in more than ten autoimmune conditions.
IL-1 is another active proinflammatory chemical, and its blocker is used for rheumatoid arthritis management and other autoinflammatory conditions with sustained favorable effects. IL-8 also plays a significant role in recruiting and activating neutrophils during inflammation.
In view of these findings, many possible immunomodulatory drugs have started being used in clinical trials and for off-label use in COVID-19. However, they have significant side effects, which mandates careful study to find biomarkers that will tell doctors when to use these drugs to maximum effect.
Identifying Cytokines that Predict COVID-19 Severity: The Study
The current study aimed to find out how and which inflammatory cytokines could help predict the course and outcome of disease in COVID-19. The researchers narrowed down their field to just four cytokines, as mentioned above - IL-6, IL-8, TNF-α, and IL-1β. The researchers tested clinically available drugs to counteract the four pathogenic cytokines, using the ELLA microfluidics platform to measure them within 3 hours.
The study included over 1,480 patients with suspected (167) or confirmed (1,257) COVID-19, in Mount Sinai hospitals, who were followed up from admission to discharge or death. At admission, all patients had their blood checked for the levels of these four cytokines. These were then correlated with disease severity, by clinical and laboratory findings, and the patient outcome.
Overall, COVID-19 patients had higher levels of IL-6, IL-8, and TNF-α than healthy controls or those on CAR-T cell therapy but without CRS. Most of the COVID-19 patients had high cytokine levels consistent with a cytokine storm, but interestingly, the concentration of each of the cytokines was not well correlated with those of the others. IL-6 showed the most significant fluctuation and IL-1β, the lowest, indeed, at the lower limit of detection.
With men, IL-6 levels were higher than for women. With the first three cytokines, levels increased with age, but not with body mass index. However, the prevalence of obesity in this group was higher. IL-1 β and TNF- α levels were significantly higher in Hispanics vs. blacks.
Chronic kidney disease (CKD) was linked to IL-8 and TNF-α. No other disease condition showed a significant association. Only age and CKD were linked to an increased risk of mortality from COVID-19. Singly, the first measurement of each cytokine was capable of predicting overall survival.
After adjusting for demographic factors and other illnesses, all except IL-1 β remained significant. Thus, patients aged over 70 had a 45% lower survival compared to those aged 50-70 years, and 76% lower compared to those below 50 years. A high IL-6 predicted a 227% increase in chances of death, and TNF- α reduced the chances of survival by 150%.
Cytokines to Predict High-Risk Patients
The researchers found strong correlations between the four cytokines and known laboratory markers of inflammation, and with fever as well in the case of IL-6 and IL-1 β. In addition, the clinical severity scale was also closely correlated with IL-6 and IL-8, which remained independent predictors of disease severity. TNF-α rose with end-organ damage.
Cytokines and Treatment Protocols
From a smaller subset of 244 patients who had repeated cytokine measurements, the researchers tested the effect of various treatments on cytokine levels. They found that treatment with the IL-6 receptor blocker tocilizumab, used in some patients with progressive respiratory failure and systemic inflammation, with high IL-6 levels, led to a transient rise in this cytokine alone, while TNF-α slowly fell.
Steroids and remdesivir caused IL-6 but not TNF-α to fall rapidly and slowly over time, respectively. No clear trend was observed with other drugs.
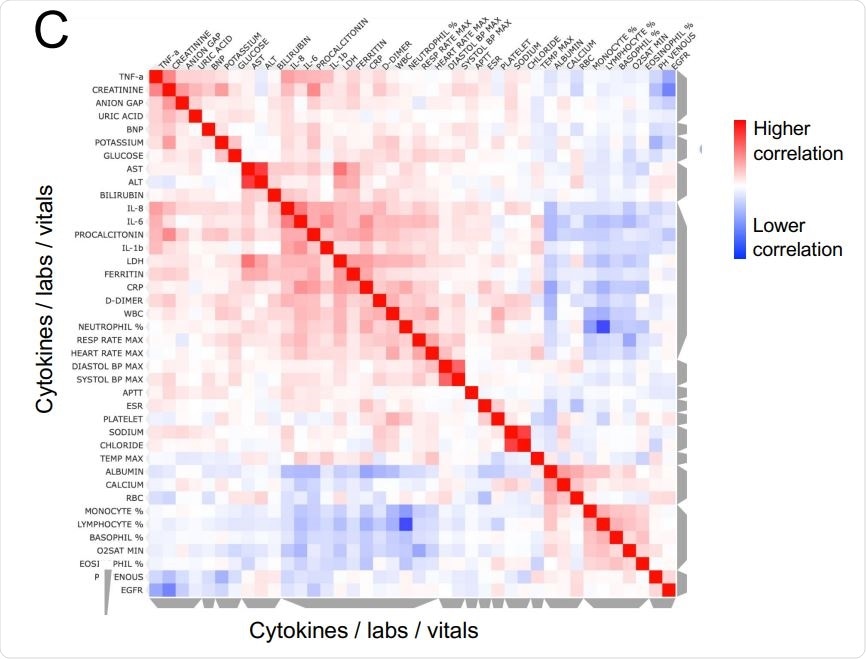
Unsupervised clustering of laboratory measurements in a subset of 1069 patients with sufficient available information. On the y axis are vitals and laboratory values after z-scoring, and on the x-axis are individual patients, using metrics measured from the time point corresponding to the first ELLA cytokine test. Grey bars on the side of the plot indicate clusters of patients or analytes, where cytokines co-cluster with known severity metrics, such as LDH, CRP, ferritin, D-dimer, but also high neutrophil, platelet and white blood counts. Annotations show patients who died in orange, and maximum severity score achieved in gray shades. B. Similarity matrix of patients based on analytes and measurements, showing two major clusters, with enrichment in patients who died and had more severe COVID-19 on the upper left. C. Similarity matrix of cytokines, lab measurements, and vitals, showing IL-6, IL-8, and IL-1b co-clustering with known inflammatory markers such as LDH, CRP, ferritin, and D-dimer, while TNF-a coclusters with organ damage markers.
Implications
The study shows that COVID-19 survival causes high levels of all four cytokines at presentation. IL-6 is among the strongest indicators of survival, more than currently used inflammatory markers like CRP or D-dimer. It can be used with markers of end-organ damage and the ventilation status to predict survival and severe disease.
TNF-α also predicts very severe disease or death even when adjusted for a host of other risk factors and for IL-6 levels.
The study also shows that the cytokine response in COVID-19 is different from that seen in sepsis and CAR-T cell therapy, with an uncoordinated and sustained cytokine response. This could point to the possibility of using specific anti-cytokine treatments to alleviate disease severity. More research must be conducted to find out which and when such therapies are useful.
In summary, the researchers found that when IL-6 and TNF- α are high at the time of admission, the patient is likely to have severe disease and reduced survival, irrespective of the use of other clinical and laboratory findings. The researchers say boldly, “These results suggest that multiplex cytokine profiling should be used to stratify patients and guide resource allocation and prospective interventional studies.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources