The global COVID-19 pandemic is caused by the Severe Acute Respiratory Syndrome 2 (SARS-CoV-2) novel coronavirus and has caused hundreds of thousands of deaths and millions of cases of the disease worldwide. Initially known for its respiratory manifestations, the other features of the disease are coming to light, including neurologic and procoagulant events.
One of these signs is delirium, which is a serious neurologic syndrome linked to many adverse outcomes in COVID-19 disease. The complications of delirium include longer duration of mechanical ventilation, of intensive care unit (ICU) stay, of hospitalization, a higher death rate, and the chances of being institutionalized after discharge.
The greater the delirium, and the longer it lasts, the higher are the chances of these outcomes. In fact, as delirium worsens, the chances of poor cognitive recovery and functional impairment become higher.
Pre-COVID-19, the prevalence of delirium in patients on mechanical ventilation was about 17% to 33%, down from a peak of about 80%. However, with the COVID-19 pandemic, hospitals and ICUs have been overwhelmed with a flood of seriously ill patients. This has inevitably strained healthcare resources and may have contributed to the return of delirium rates in the ICU setting to their former levels.
This was illustrated by a small French study that quoted a rate of delirium at about 65% in ICU patients. If this is the case with ICU patients in the US as well, of whom there are tens of thousands at present, delirium may well result in a long-term requirement of care for many patients, with the inevitable burden on the public health system.
This study was carried out at two large hospitals in the US Midwest and was aimed at the incidence, duration, and severity of delirium as well as the risk factors for delirium in critically ill COVID-19 patients.
There were 144 patients eligible for the study out of 243 consecutive confirmed COVID-19 patients admitted between March 1, 2020, to April 27, 2020. All of them were discharged from the ICU by the end of the study. The mean age was 58 years, and 58% of them were male. About half of them were blacks and 14% Hispanic.
About 60% of them had hypertension, 56% obesity, 27% used tobacco, and 26% had chronic lung disease. Almost three-fourth of patients required invasive mechanical ventilation. Only about 1% had any evidence of stroke.
Delirium Incidence
In the current study, delirium was identified through the Confusion Assessment Method for the ICU (CAM-ICU). This score looks for mental status fluctuations or changes, loss of attention, reduced consciousness, or lack of organized thinking.
The researchers found that about 74% had delirium, typically setting in within the first two days of ICU admission. If coma was also considered, it came to about 76%. About 63% were diagnosed to have coma at the first evaluation, and 37% on the second.
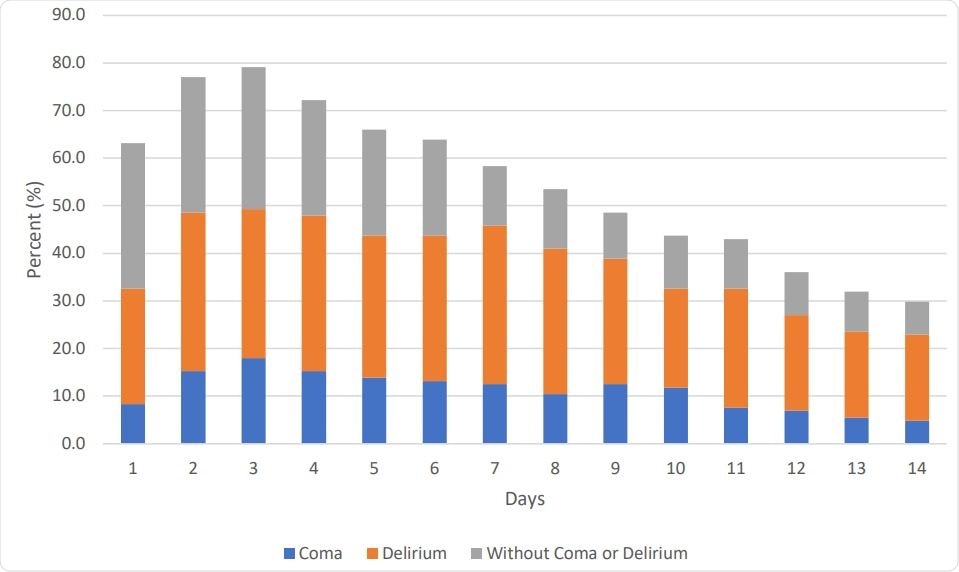
Daily Rates of Delirium, Coma, or Without Delirium/coma Status as Assessed up to First 14 Days of Intensive Care Unit Stay (n=144)

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The severity of illness is typically evaluated using the Acute Physiology and Chronic Health Evaluation Score (APACHE-II). This is calculated using laboratory values, vital signs, and neurologic assessments performed in the first 24 hours of ICU admission.
Delirious patients in the current study had a higher APACHE-II score for severity of illness at admission and were far more likely to be on a ventilator, at 91% vs. 21%. They were more likely to be hypoxemic, had lower levels of consciousness in the first 24 hours in the ICU, as well as over the 14 days of ICU stay.
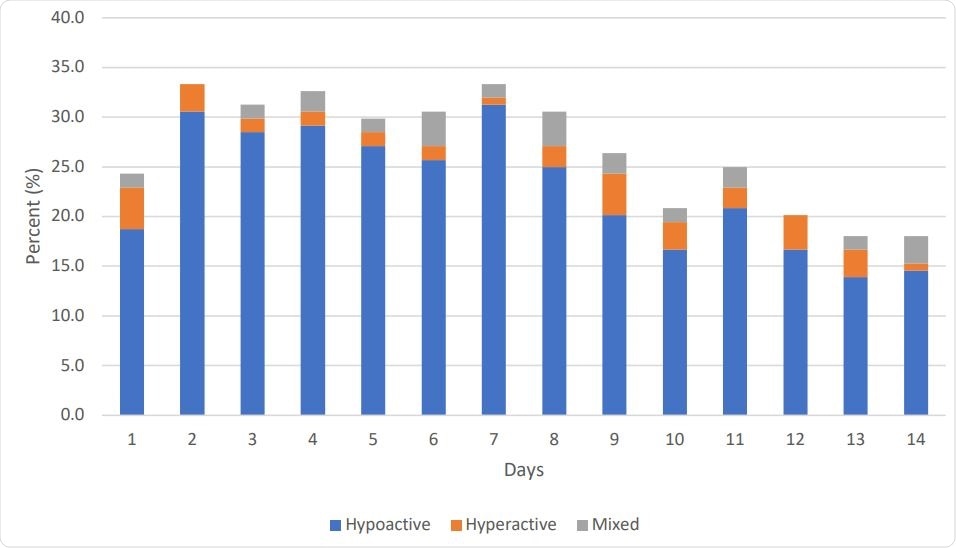
Subtypes of Delirium in Critically Ill Patients with COVID-19 Who Developed Delirium (n=106)
Delirium Duration and Severity
The median duration of delirium and coma was 7 days, while for delirium alone, it was 5 days. The median level of consciousness was light sedation. Factors associated with delirium included:
- Greater number of days on the ventilator compared to non-delirious patients (median: almost 9 days vs. 0 days)
- Greater number of ICU days (median 11 vs. almost 4 days)
In this study, the severity of delirium was measured in 73 patients, showing a median score of 6 on the Confusion Assessment Method for the Intensive Care Unit-7 (CAM-ICU-7), indicating severe delirium.
The researchers found that being on mechanical ventilation was increased with an astronomical 42-fold rise in the odds of delirium. However, the study sample was too small to be able to pick up an increase in mortality rates.
The study findings are not in agreement with many other recent publications on delirium in ICU patients during the latest influenza outbreak. In fact, earlier studies at one of the same centers showed a 36% rate of mechanical ventilation, a 23% rate of delirium, and a 24% rate of coma during that period.
Causes of COVID-19-Related Delirium
What could have pushed up delirium rates in the COVID-19 period? The researchers assume that better clinical guidelines and multidisciplinary regimens for the prevention of delirium, and the use of techniques that reduce the rates of invasive mechanical ventilation, in addition to increased awareness of the dangers of delirium, have all contributed to a dramatic reduction in ICU delirium.
The stress of the ongoing pandemic, and especially the abrupt influx of large numbers of critically ill patients into ICUs, disrupted these clinical routines leading to an inability to apply such care improvements. Moreover, some think that direct viral injury to the central nervous system may cause delirium. These theories require more study to elucidate the neural and other pathways underlying the development of delirium.
The study concludes, “Our study sheds light on an alarming burden of delirium and coma in patients admitted to the ICU and the need for continued efforts on delirium prevention.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources