An international team of researchers reports that patients with coronavirus disease 2019 (COVID-19) release thousands of viral particles directly into the air simply though breathing.
The researchers say the patients in the study exhaled severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) at an estimated rate of up to 100,000 particles per minute.
“A COVID-19 patient exhales millions of SARS-CoV-2 particles per hour,” say Maosheng Yao (Peking University, Beijing) and colleagues.
The researchers say that currently, the main transmission routes are generally thought to be exposure to respiratory droplets and direct contact transmission.
However, they add that their study found the likelihood of SARS-CoV-2 existing on the surfaces of objects commonly used by COVID-19 patients was very low.
The researchers suggest that exhaled breath may be the primary SARS-CoV-2 shedding mechanism and warn that it is crucial to protect against airborne transmission by increasing the use of ventilation systems and face masks.
A pre-print version of the paper is available in medRxiv* while the article undergoes peer review.
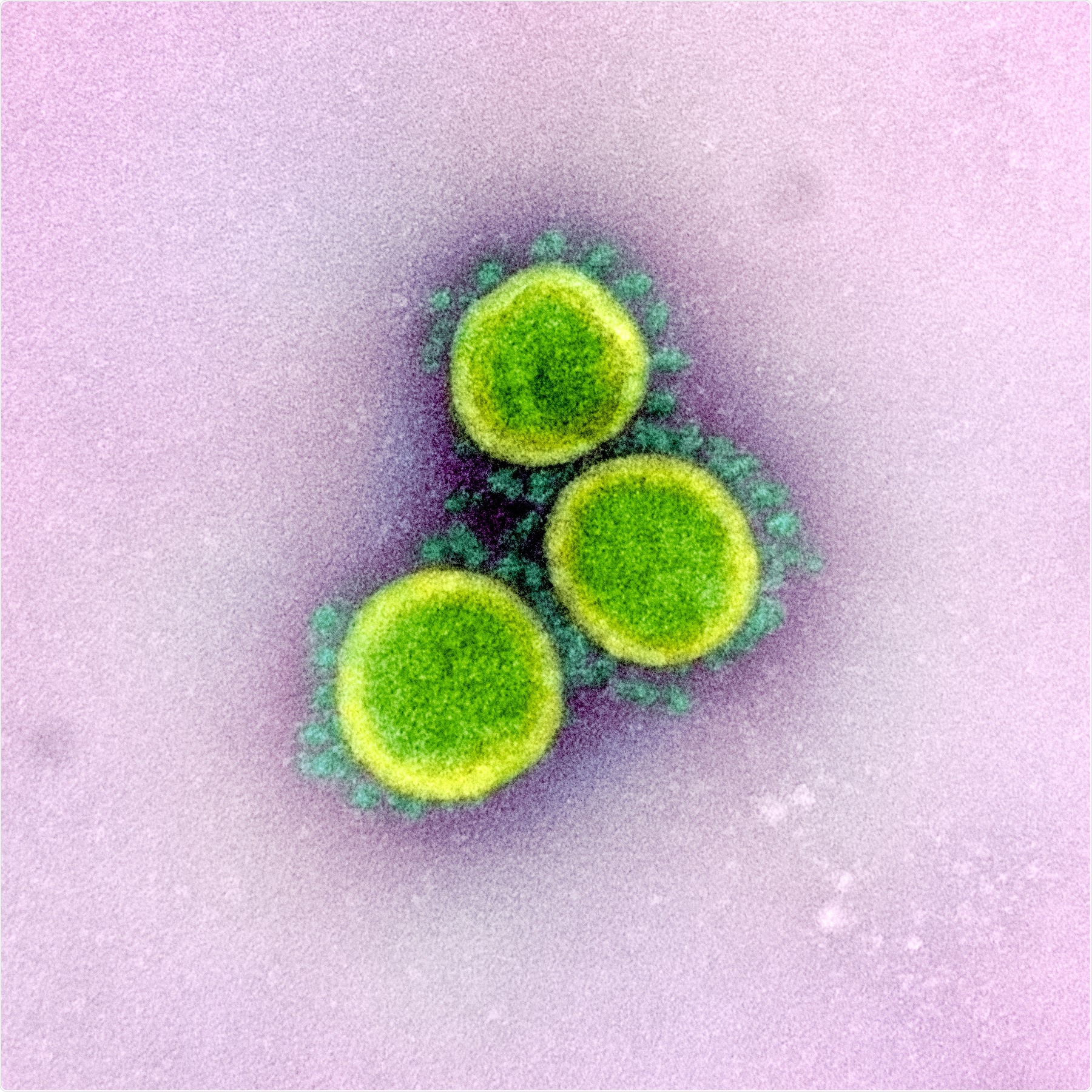
Novel Coronavirus SARS-CoV-2 Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Debate surrounding modes of transmission
Although considerable efforts have been made worldwide to slow the spread of SAR-CoV-2, researchers still need to understand more about the main routes of transmission.
The virus has been detected in the air, on cell phones, patients’ hands, hospital floors, and ventilation units. Some studies have also shown that aerosolized virus particles survive on surfaces for sustained periods and remain viable in the air for as long as three hours.
However, experts are still divided over the main routes of transmission, and no clear evidence has yet emerged describing how SARS-CoV-2 is emitted into the air.
Now, Yao and the team have explored the main potential transmission routes by collecting and analyzing 298 samples from 35 COVID-19 patients. Thirty of the samples collected were exhaled breath condensate (EBC), all of which were taken within less than 14 days since symptom onset; 26 were air samples, and 242 were surface swabs.
What did the researchers find?
On analyzing the EBC samples, the researchers detected SARS-CoV-2 in five patients, all of whom were aged under 50 years. Of those five patients, one had a cell phone and hand swabs that tested negative for the virus, but a toilet pit swab taken from their hotel room that tested positive. Another patient had a swab taken from the ventilation duct beneath the bed in their ward that tested positive.
Overall, the SARS-CoV-2 detection rate among EBC samples was 16.7%.
“Our data reveal direct evidence of airborne transmission of SARS-CoV-2 via breathing,” writes the team. “The exhaled SARS-CoV-2 could be partially responsible for the contamination on the surfaces that were observed.”
Of the 26 air samples taken, only one sample tested positive, giving an overall SARS-CoV-2 positivity rate of 3.8%. The air sample was taken from the patient’s unventilated quarantine hotel room. A surface swab of a ventilation duct in the room also tested positive.
The researchers point out that although the rate of SARS-CoV-2 positivity was low among the air samples, the data still shows that the air space of an environment housing COVID-19 patients was contaminated with the virus.
Of the 242 surface swab samples, 13 tested positive for SARS-CoV-2 across five types of surface. Toilet pits had the highest positivity rate, at 16.7%, and the hospital floor had the second-highest rate, at 12.5%. This was followed by other surfaces (those shared by patients, medical staff, or visitors; 7.4%); patient touching surfaces (those frequently touched by the patients; 4.0%), and medical touching surfaces (those frequently touched by the medical staff; 2.6%).
The authors were surprised to find that only two of 22 cell phone swabs tested positive for the virus and that none of 26 swabs collected from the handles of various items tested positive.
The overall SARS-CoV-2 positivity rate among surface swabs was 5.4%.
“These observations do not support the widely-held belief that direct transmission by contact with surfaces plays a major role in COVID-19 spread,” says Yao and colleagues.
Exhaled emission may be the main viral shedding mechanism
“For the first time, we here report that the SARS-CoV-2 is released directly into the air via breathing by COVID-19 patients,” write the researchers.
The team estimates that the exhaled emission rate of SARS-CoV-2 was about 1,000 to 100,000 virus particles per minute, with the highest rate seen during the early stages of COVID-19.
“Most SARS-CoV-2 in exhaled breath should fall in the fine aerosol size (<2.5µm) ranges, which can remain airborne for a far longer time than the coarser ones emitted otherwise in a sneeze or cough,” said Yao and colleagues.
Furthermore, the mobile phones and various handles commonly used by the patients in this study were very unlikely to be contaminated with SARS-CoV-2, they add.
“Evidence from our work shows that exhaled breath emission may well be the most significant SARS-CoV-2 shedding mechanism,” write the researchers.
“Accordingly, measures such as enhanced ventilation and the use of face masks are essential to minimize the risk of infection by airborne SARS-CoV-2,” they conclude.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.