The researchers wrote that antimicrobial resistance is one of the most significant health problems that humans face today. Infections that could once be treated effectively with antibiotics are increasingly becoming difficult to treat owing to the emergence of antibiotic resistance by bacteria. Indiscriminate use and overuse of antibiotics are some of the significant reasons behind the emergence of such antibiotic resistance.
A new drug Teixobactin is one of the first of its class and is being developed naturally from a soil bacteria called Eleftheria terrae. This drug was discovered in 2015 by Professor Kim Lewis at Northeastern University in Boston and colleagues.
To date, this bacteria remained un-culturable in the laboratory, wrote the researchers. Teixobactin has been shown to be effective against both MRSA and VRE. This antibacterial agent has been shown to be immune to the development of resistance by microbes, wrote the researchers. This study looked at the mechanism by which Teixobactin achieves this.
The authors of this new study from the University of Melbourne, wrote, “The cyclic depsipeptide teixobactin holds much promise as a new class of antibiotics for highly resistant Gram-positive pathogens (e.g., methicillin-resistant Staphylococcus aureus [MRSA]). Understanding its molecular mechanism(s) of action could lead to the design of new compounds with a broader activity spectrum.”
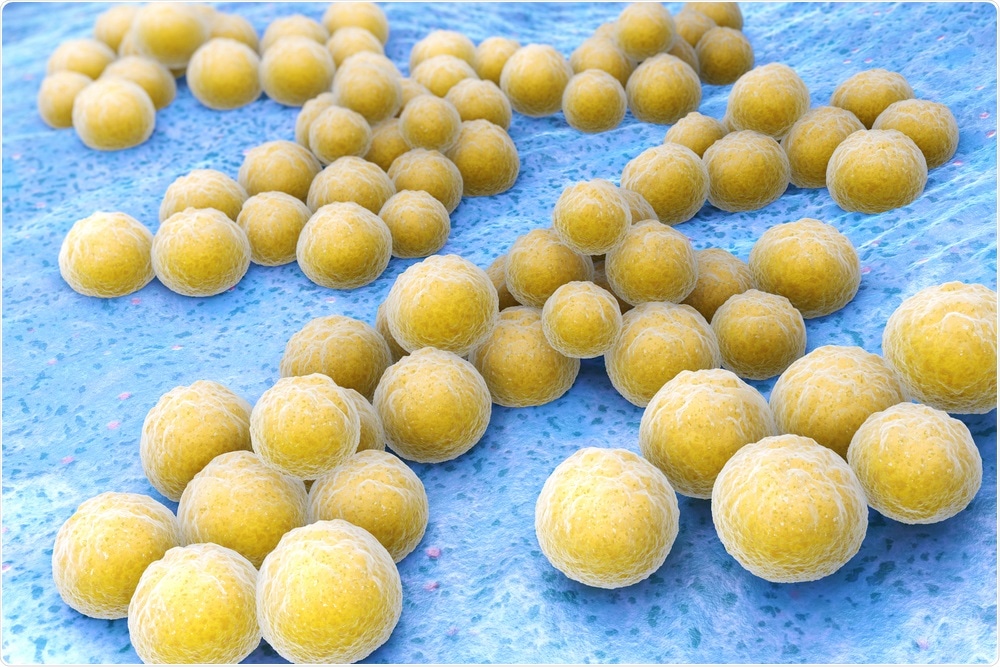
Methicillin-resistant Staphylococcus aureus (MRSA). Image Credit: Tatiana Shepeleva / Shutterstock
What was done?
The researchers speculated that this “resistance-resistant” mechanism of action of Teixobactin included its capacity to bind to lipid II and lipid III. These molecules are building blocks of the bacterial cell wall. The team used metabolomics to look at the metabolic pathways that could allow this antibacterial agent to resist the resistance caused by bacteria.
The researchers used a synthetic teixobactin analog Leu10-teixobactin. It was used against an MRSA strain, S. aureus ATCC 700699. The bacterial cell metabolomes were treated with the drug, and another control group was left untreated. The effect of the Teixobactin was checked at 1, 3, and 6 hours. The concentration of the test drug used was 0.5 μg/ml, i.e., 0.5× MIC (Minimum Inhibitory Concentration).
For this study, a team including research fellow Dr. Maytham Hussein and Associate Professor Tony Velkov developed a synthetic form of Teixobactin. According to Dr. Hussein, MRSA is typically a challenge, and it is challenging to prevent the development of resistance against this organism. He said, “The rise of multidrug-resistant bacteria has become inevitable. These bacteria cause many deadly infections, particularly in immunocompromised patients such as diabetic patients or those with cancers, or even elderly people with post-flu secondary bacterial infections.”
What was found?
Results showed that Leu10-teixobactin damaged the membrane lipids that coated the bacteria, including glycerophospholipids and fatty acids. It also affected the peptidoglycan (lipid I and II) metabolism as well as the biosynthesis of cell wall teichoic acid (lipid III). These effects of the drug helped kill the bacteria and also prevented resistance development.
The effects were noted during the first hour of treatment. The team said that this meant that the Teixobactin was working on the cell envelope to start with. The bacterial killing was time-dependent, they wrote. The drug was also found to interfere with the metabolic pathways of the bacterial cell, including amino-sugar and nucleotide-sugar metabolism. At 3 and 6 hours reading, it could affect the peptidoglycan and teichoic acid biosynthesis. The drug was also found to significantly interfere with other metabolic pathways of the bacteria such as, “arginine metabolism and the interrelated tricarboxylic acid cycle, histidine metabolism, pantothenate, and coenzyme A biosynthesis”. These were noted at 3 and 6 hours after drug treatment.
Conclusions and implications
This was the first study to show that Teixobactin had a novel effect on the metabolic pathways of drug-resistant bacteria. The team wrote that this study “lends support to the development of teixobactin as an antibacterial drug for the treatment of multidrug-resistant Gram-positive infections.” They added, “These novel results help explain the unique mechanism of action of teixobactin and its lack of cross-resistance with vancomycin.”
Associate Professor Tony Velkov, in his statement, said, “Our published data will greatly facilitate the pre-clinical development of teixobactin. It holds much promise as a ‘resistant to resistance’ antibiotic for the highly resistant Gram-positive pathogens such as MRSA. These novel results will open doors to develop novel antibacterial drugs for the treatment of multi-drug resistant Gram-positive infections which are caused by certain types of bacteria.” Hussein added that since this is an FDA approved compound, the process of development of this drug is faster. He said, “The FDA-approved compounds have already passed all safety measures with a known toxicity profile, so we basically save time and cost. Drug development is a very complex process, especially when developing new antibiotic classes that fit the criteria of being highly active, having acceptable pharmacokinetic properties, and being reasonably safe.”
Journal reference:
- The Killing Mechanism of Teixobactin against Methicillin-Resistant Staphylococcus aureus: an Untargeted Metabolomics Study Maytham Hussein, John A. Karas, Elena K. Schneider-Futschik, Fan Chen, James Swarbrick, Olivia K. A. Paulin, Daniel Hoyer, Mark Baker, Yan Zhu, Jian Li, Tony Velkov mSystems May 2020, 5 (3) e00077-20; DOI: 10.1128/mSystems.00077-2, https://msystems.asm.org/content/5/3/e00077-20