The researchers identified three cytokines by using a new strategy to construct a model that differentiated between healthy individuals, asymptomatic carriers of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and COVID-19 patients with non-severe disease.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
However, the model was not effective at distinguishing patients with severe disease.
After further adjusting the new strategy, the researchers eventually identified a single cytokine called human hepatocyte growth factor (HGF) that could distinguish between severe and non-severe COVID-19, with high sensitivity and specificity.
Ai-Long Huang and colleagues suspect this may be because HGF only increases significantly once inflammation is approaching the life-threatening stage of a cytokine storm.
The authors say that as well as having identified a potential new treatment for severe COVID-19, the new strategy could help pinpoint cytokine biomarkers of infectious disease states and provide a new way to probe the modulation of cytokines involved in the immune response.
A pre-print version of the paper is available in medRxiv*, while the article undergoes peer review.
Inflammation is an important factor in COVID-19
The COVID-19 pandemic, which began in Wuhan, China late last year, has now reached every corner of the world and infected more than 6 million people.
The disease is caused by infection with the highly transmissible SARS-CoV-2, which uses the host cell receptor angiotensin-converting enzyme 2 (ACE2) as a receptor to gain entry to cells.
Human alveolar epithelial cells express high levels of ACE2, making the lungs a susceptible target, and infected patients generally experience lower respiratory tract symptoms such as dry cough and sometimes difficulty breathing.
To some degree, these symptoms reflect inflammation in the lungs, which is caused by the host immune responses to viral infection. The triggering of these immune responses can generate cytokines that, in turn, trigger a proinflammatory response that attracts white blood cells such as macrophages and neutrophils to infection sites.
Once having reached the infection sites, these phagocytes can then damage healthy tissue when they release cytotoxic substances. Research has shown that the levels of some cytokines are significantly increased in cases of COVID-19, and that cytokine storms are associated with severe disease.
Using cytokines to predict disease state
Now, Huang and the team have used a new strategy to screen cytokine biomarkers of COVID-19 by considering the fluctuations in and relationships between cytokines. These factors have generally been overlooked in other studies.
The new strategy identified cytokines that can classify populations in the different states of disease caused by infection with SARS-CoV-2.
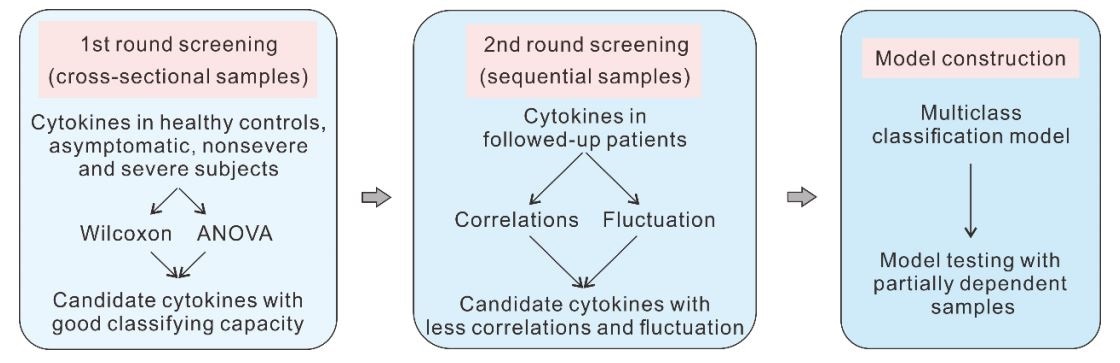
Strategy for screening cytokine biomarkers of COVID-19
These cytokines were first screened in cross-sectional serum samples obtained from 184 participants, including 37 healthy people, 37 asymptomatic SARS-CoV-2 carriers, 97 COVID-19 patients with the non-severe disease, and 13 patients with severe disease.
The inter-relationships and fluctuating characteristics of these cytokines were then analyzed in sequential serum samples obtained from 38 COVID-19 patients.
The team eventually narrowed down potential cytokine biomarkers to three candidates, namely macrophage colony-stimulating factor (M-CSF), interleukin (IL)-8, and stem cell factor (SCF), which were then used to construct a multiclass classification model.
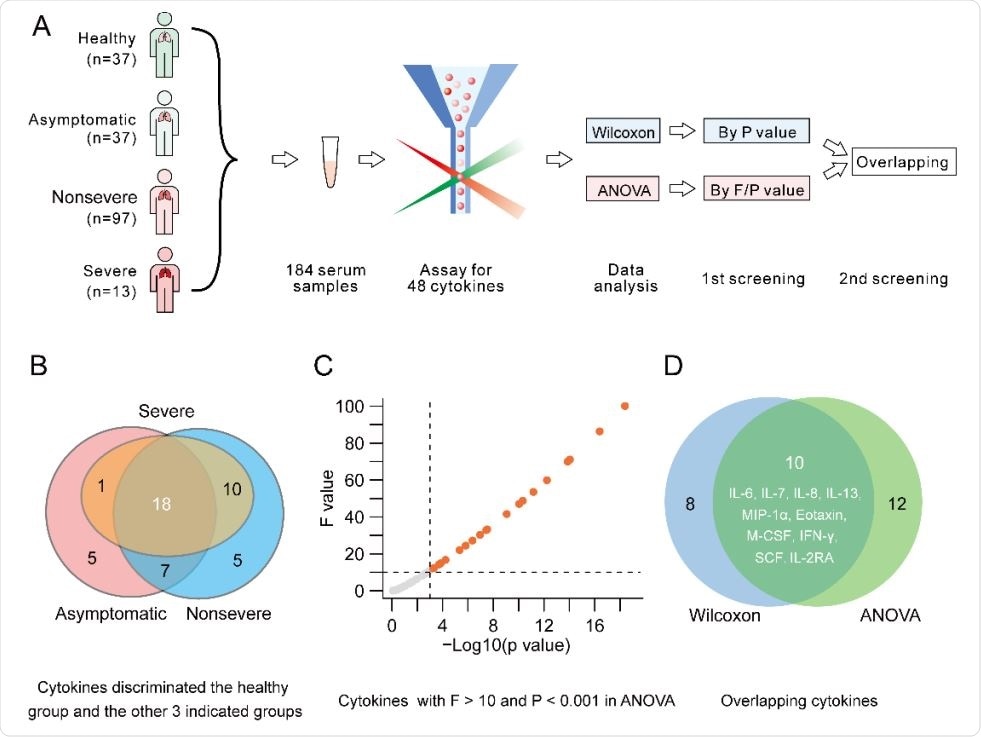
Preliminary screening of cytokines. A. Procedure of preliminary screening of candidate cytokines. B. Cytokines with the potential to discriminate the healthy control group and the other 3 groups. C. Cytokines with F > 10 and P < 0.01 in ANOVA. D. Overlapping cytokines meeting the criteria of the 2 statistical analyses.
How did the model perform?
The model differentiated between healthy people, asymptomatic individuals, and non-severe disease, with an accuracy of 77.4%.
However, the model could not accurately distinguish patients with severe disease (1.7%), which the authors say indicates “the difficulty in finding cytokines that can discriminate the entire spectrum of COVID-19 simultaneously.”
The team then adjusted the cytokine searching strategy by screening for cytokines that only differed significantly between patients with the severe and non-severe disease.
This led them to a single cytokine – HGF – that could distinguish severe patients form non-severe ones with a sensitivity of 84.6% and specificity of 97.9%.
The HGF level was not elevated in patients with non-severe disease but was elevated among those with severe disease.
Increased HGF may be “consequence of excessive inflammation”
“HGF is a potent anti-inflammatory factor that ameliorates inflammation and dysfunction in a wide variety of experimental animal models. It inhibits inflammation by interfering with proinflammatory NF-κB signaling,” explain Huang and colleagues. “Considering its function, the increase in HGF in severe COVID-19 must not be a reason for but rather a consequence of excessive inflammation.”
They also suggest that the HGF level may only increase significantly once inflammation is approaching the cytokine storm stage, in which case it may be considered a dampener of this hyperinflammatory state and, therefore, a candidate therapy for critical cases of COVID-19.
“In addition, our new strategy provides not only a rational and effective way to focus on certain cytokine biomarkers for infectious diseases but also a new opportunity to probe the modulation of cytokines in the immune response,” the team concludes.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.