“To our knowledge, this is the first study to report an association between plasma RNLS [renalase] levels and COVID-19 severity,” writes Gary Desir and colleagues.
The researchers say that the use of renalase agonists should be investigated for its potential value as a therapy for severe COVID-19.
The study, which involved 51 adult patients hospitalized with COVID-19, also found that all patients treated with the antiviral remdesivir required admission to ICU, suggesting that the use of this drug is associated with more severe disease.
Remdesivir was initially developed as a treatment for hepatitis C and tested as a therapy for Ebola, but was not effective at treating either virus. However, it has recently been tested as a therapy for COVID-19, and in some countries, it has been authorized as an emergency treatment.
A pre-print version of the research paper is available on the server medRxiv*, while the article undergoes peer review.
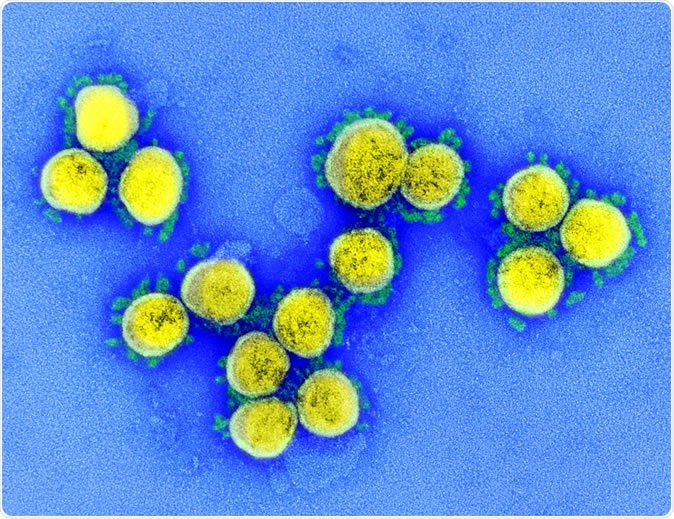
SARS-CoV-2 - Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Validated markers of disease progression are needed
Since the COVID-19 outbreak began in Wuhan, China, late last year, the virus is now reported to have infected around 6.9 million people and to have caused about 400,000 deaths. The disease ranges in severity from asymptomatic to severe, with patients developing extensive lung damage and a dangerous hyperinflammatory state called “cytokine storm syndrome.”
“Validated markers of disease progression could affect management and therapy,” say Desir and team.
How might renalase be involved in COVID-19?
Renalase is a flavoprotein secreted into the blood by the kidneys. The enzyme has been shown to exert potent anti-inflammatory activity across a range of disease processes, and it is associated with increased survival.
According to the authors, in cases of acute kidney injury and acute pancreatitis, a low blood renalase level results in increased organ inflammation and injury.
Disordered inflammatory responses, increased inflammation, decreased T-cell activity, and cellular injury is central features of COVID-19 pathogenesis, and hyperinflammation has been shown to be associated with severe disease.
Since renalase is known to reduce tissue inflammation, Desir, and colleagues hypothesized that the blood renalase level may serve as a biomarker of disease severity among patients with the illness.
What did the study involve?
The team assessed blood levels of renalase and inflammatory cytokines among 51 COVID-19 patients hospitalized at Yale New Haven Hospital between March 1 and April 23 and compared them with levels among 15 uninfected control subjects. They also assessed sociodemographic and clinical information available in medical records.
Of 39 patients admitted to ICU, thirty (80%) were receiving mechanical ventilation at enrollment, and the other 12 patients were receiving oxygen supplementation.
Among the COVID-19 patients, the renalase level ranged from 1,964 ng/mL to 22,675 ng/mL (median of 7,144 ng/mL) and the cut-off value for those in the lowest quartile was 5,522 ng/mL.
Lower renalase levels were associated with less likelihood of survival
After adjustment for confounding factors such as age, gender, comorbidity, and steroid use, the plasma renalase level was inversely associated with the inflammatory cytokines interleukin (IL)-1β, IL6, and tumor necrosis factor-alpha (TNFα), but not with interferon-gamma (IFNγ).
Patients with COVID-19 had significantly lower renalase levels than the controls, and low renalase was associated with increased disease severity and a 4.5-fold increased risk for worse overall survival.
The proportion of patients with COVID-19 who required mechanical ventilation was significantly higher among those with a low renalase level than among those with a high level, at 84.6% compared with 50.0%.
Patients receiving remdesivir
Patients with a low renalase level were more likely to be receiving remdesivir, compared with patients who had a high renalase level, and all patients taking remdesivir were admitted to the ICU.
The team says this suggests that “remdesivir use in our cohort likely correlated with more severe COVID19 disease.”
What are the implications of the study?
“Plasma RNLS may be useful as an additional biomarker to identify patients with more severe disease and alludes to a potential pathophysiological mechanism associated with inflammation in COVID-19 disease,” say Desir and colleagues.
“Accordingly, the potential therapeutic value of RNLS agonist administration in patients with severe COVID-19 should be examined,” concludes the team.
Gary Desir is a named inventor on several issued patents related to the discovery and therapeutic use of renalase. Renalase is licensed to Bessor Pharma, and Gary Desir holds an equity position in Bessor and its subsidiary Personal Therapeutics.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources