Researchers in Italy have found that it is possible to completely inactivate severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) using short-wavelength UV (UV-C) irradiation.

Surgical mask is irradiated by UVC (ultraviolet C) light. Image Credit: SMPTY 17 photography mos / Shutterstock
At a viral concentration equivalent to the low-level found in settings such as hospital rooms and to the level typically found in the sputum of coronavirus disease 2019 (COVID-19) patients, a very low dose of UV-C radiation was sufficient to inactivate SARS-CoV-2 completely.
At a viral input equivalent to that found in terminally ill patients, a higher dose of radiation also completely inactivated the virus.
Mario Clerici (University of Milano) and colleagues say that since UV light from the sun seems to be effective at inactivating the virus, the findings could explain trends observed in the distribution, incidence, and spread of SARS-CoV-2.
The results also have extremely important implications for the design and development of effective sterilization methods for containing SARS-CoV-2, they add.
A pre-print version of the paper is available on the server medRxiv*, while the article undergoes peer review.
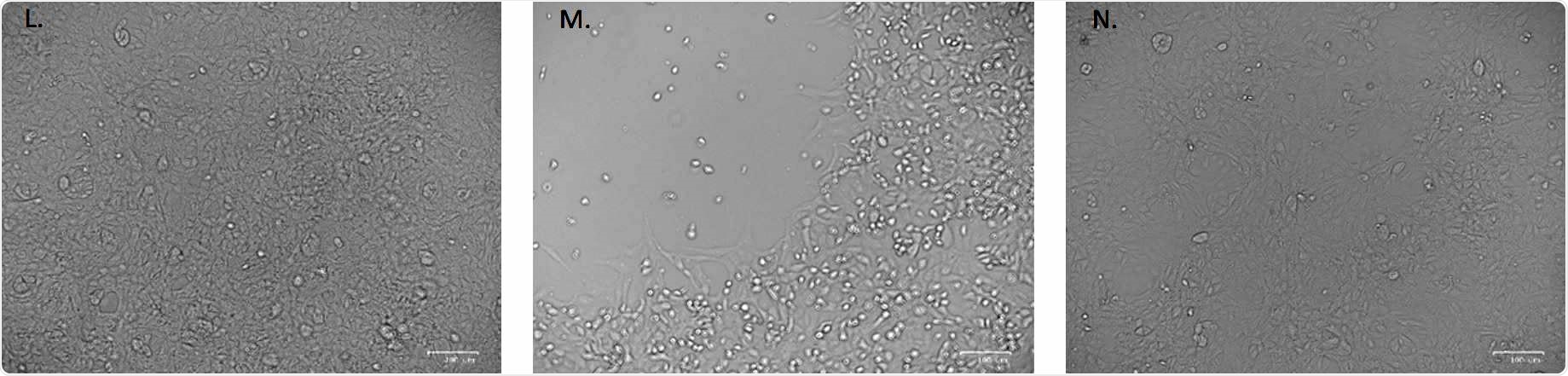
No cytopathic effect was observed in uninfected cultured VeroE6 monolayers maintained in 50mJ/cm2 UVTtreated complete medium for 72 hours. (M) In vitro infection of SARSTCoVT2 (5 MOI) UVTC untreated VeroE6 cells resulted in an evident cytopathic effect. (N) SARST CoVT2 irradiation with 3.7 mJ/cm2 UVTC rescued the cytopathic effect induced by UVTC untreated virus.
Disinfection technologies are urgently needed
Since its outbreak in Wuhan, China, in December last year, the COVID-19 pandemic has had a devastating impact on people's health globally and the world's economic outlook.
Clerici and colleagues say the identification of "microbicide" methods that will minimize any future spread of SARS-CoV-2 is essential since the virus can survive outside of the body in the air for hours.
"In this context, non-contact disinfection technologies are highly desirable, and UV radiation, in particular UVC (200 – 280 nm), is one of the most reliable and widely accepted approaches," writes the team.
According to the authors, many studies have explored how UV-C radiation destroys viruses, and the most common mechanism is "direct absorption of the UV-C photon by the nucleic acid basis or capsid proteins leading to the generation of photoproducts that inactivate the virus."
Several models have been proposed to help understand the UV-C radiation doses required to achieve viral inactivation, but the authors say no reliable model is in the pipeline yet. This is partly because experiments have been conducted using different viruses and different experimental conditions, resulting in wide-ranging dosage values being reported for the same viruses, says the team.
In the case of SARS-CoV-1 for example, the dosages reported have ranged from just a few millijoules (mJ) per cm2 to hundreds per cm2.
In the meantime, it is essential to have direct evidence of disinfection, and the corresponding doses required for inactivation and inhibition of SARS-CoV-2 says the team.
What did the study involve?
Using a low-pressure mercury lamp system, the team administered different UV-C doses (3.7, 16.9 and 84.4 mJ/cm2) to SARS-CoV-2 at a multiplicity of infection (MOI) of 0.05 (equivalent to low-level contamination); 5 (equivalent to the level in sputum from COVID-19 patients) and 1000 (equivalent to the level in cases of terminal disease).
Following exposure to UV-C radiation, viral replication was measured by applying real-time polymerase chain reaction (PCR) to regions of the nucleocapsid gene and by assessing virus-induced cytopathic effects.
At low and intermediate contamination levels, a very small dose of UV-C inactivated the virus
At the lowest MOI (0.05), viral replication was wholly inhibited after six days, even at the low UV-C dose of 3.7 mJ/cm2.
At the intermediate contamination level (MOI of 5), viral replication was effectively reduced by this low dose after 24 hours and did not increase over time, indicating a complete inactivation of the virus. Evaluation of cytopathic effects also confirmed virus inactivation.
A higher dose was required for the highest contamination level
At the highest viral input (MOI of 1000), viral replication significantly decreased in a dose-dependent manner after 24 hours. Still, after 48 hours, viral concentration started to increase at the lowest UV-C exposure.
However, viral concentration did not increase after 48 hours, once SARS-CoV-2 was exposed to the higher radiation doses (16.9 and 84.4 mJ/cm2).
The authors say the study shows that UV-C radiation achieves both inactivation and inhibition of SARS-CoV-2 in a dose-dependent manner.
At a viral density comparable to that of low-level contamination and to that of sputum from COVID-19 patients, a minimal dose of less than 4 mJ/cm2 was enough to inactivate the virus, say the researchers fully.
"Even at the highest viral input concentration (1000 MOI), viral replication was totally inactivated at a dose >16.9 mJ/cm2," they add.
"These results could explain the epidemiological trends of COVID-19 and are important for the development of novel sterilizing methods to contain SARS-CoV-2 infection," concludes the team.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources