The study, which focused on frontline staff working in acute hospital settings in London, has important implications for managing an anticipated “second wave," during which hospital admissions are expected to soar again, say Eleni Nastouli and colleagues.
The findings are preliminary one-month follow-up results from the early stages of a three-month longitudinal analysis of acute NHS hospital trusts in London and Liverpool.
They could help to inform decisions about the roll-out of potential vaccination programs, for example, applicable to any similar sizeable inner-city hospital.
A pre-print version of the paper is available on the server medRxiv*, while the paper undergoes peer review.

Image Credit: Paul Nicholas UK / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Higher incidence of SARS-CoV-2 among healthcare workers
In Wuhan, China, where coronavirus disease 2019 (COVID-19) was first identified, the incidence of SARS-CoV-2 was found to be higher among healthcare workers than among the general population.
Despite the measures taken in many countries to contain the pandemic, including in the UK, healthcare facilities have been implicated as settings where asymptomatic infection and transmission is ongoing.
This prompted the UK government to make personal protective equipment (PPE) compulsory for all patient contact. Although the incidence of new COVID-19 cases did start to fall once lockdown measures were introduced, only one small study has reported on any possible effect that these PPE recommendations may have had.
Furthermore, although the risk to healthcare workers and patients is clear, longitudinal data on seroconversion and evidence of SARS-CoV-2 RNA in seropositive and seronegative individuals is lacking, say Nastouli and team: “There is little description of their longitudinal antibody response in the presence or absence of SARS-CoV-2 and symptoms.”
What has the current study involved?
Two-hundred frontline staff (aged a median of 34 years) working at University College London Hospitals who met asymptomatic criteria were enrolled between 26th March and 8th April.
Participants included nurses, doctors, physiotherapists, healthcare assistants, porters, caterers, and housekeeping staff working in high-risk settings, including Accident and Emergency, acute medical admissions, COVID-19 cohort wards, Intensive Care Units, and hematology wards.
At baseline, participants provided blood samples and nose and throat swabs and self-reported demographic data and information on comorbidities, patient contact, and aerosol-generating procedures (AGPs).
Over a one-month follow-up period, the participants provided self-collected swabs and blood samples and further information about symptoms, patient contact, and AGPs twice a week.
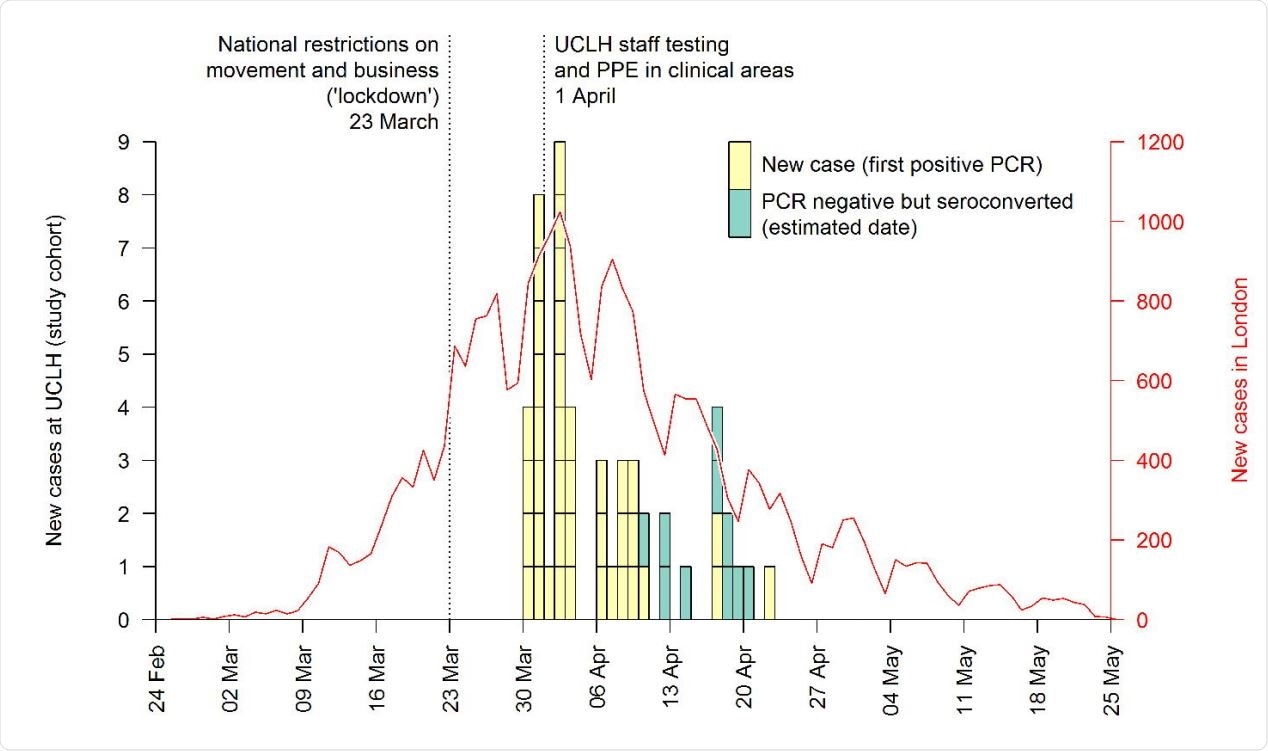
Epidemiological curve of daily confirmed cases of SARS-CoV-2 in front line health care workers at the hospital, and reported cases in London. PCR negative participants who seroconverted are shown at the midpoint between baseline and follow-up serology tests.
What did the study find?
During the one-month follow-up period, 42 (21%) of the 200 staff tested positive for SARS-CoV-2 by polymerase chain reaction (PCR). Eight of them had symptoms that met the current case definition (cough, fever, or altered taste or smell). None were ill enough to require hospital admission.
Of 181 participants who provided blood samples at baseline and during follow-up, 82 (45.3%) were seropositive for SARS-CoV-2 by early May. This included 46 who were already seropositive at baseline and 36 who had seroconverted during the study.
The team also found that of all participants who tested PCR-positive for infection, only one did not developed antibodies.
“The single HCW who was seronegative had antibodies checked 17 days after their positive swab so may not have had sufficient time to seroconvert,” explains the team.
Among participants who had antibodies at baseline, none showed evidence of re-infection during the follow-up period: “Our cohort provides limited early evidence of a lack of re-infection in the first month of follow up in those seropositive, with further data to follow.”
London healthcare workers are at particularly high risk
The researchers say other studies have reported a high level of SARS-CoV-2 infection among hospital staff, with one seroprevalence study of 578 people working in a large hospital in Barcelona indicating a SARS-CoV-2 prevalence of 11%.
“At the time of writing, London has had the highest numbers of COVID-19 hospitalizations and deaths in the country, which may account for the higher infection levels seen in London HCWs,” suggests the team.
Nastouli and colleagues warn that the high infection rate among London healthcare workers shows the high risk this group is at and how this highlights the importance of a recent government recommendation that all asymptomatic healthcare workers are screened.
“We report early results from a closely observed cohort of front line HCWs who worked throughout the peak of COVID-19 in central London and have the highest seroprevalence in HCWs published to date,” says the team.
Implications for the expected “second wave”
“This has implications for the expected ‘second wave’ during which hospital admissions are likely to increase again and is applicable to similar large inner-city hospital settings,” writes Nastouli and colleagues.
The researchers say that given the number of vaccine trials taking place, the findings could be useful for planning approaches to potential vaccination roll-out.
“Finally, the high rate of infection combined with further evidence of asymptomatic carriage of virus highlights the importance of appropriate PPE use and strengthens calls for regular surveillance with swabs in HCWs,” concludes the team.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources