The coronavirus disease (COVID-19) targets people who are at higher risk, such as the elderly, those with underlying health conditions, and those who have weakened immune systems. In severe cases of COVID-19, damage can spread beyond just the lungs and into other organs, including the heart, kidneys, liver, and the brain.
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) uses the enzyme angiotensin-converting enzyme 2 (ACE2) to enter and infect human cells. It causes COVID-19 and can lead to a multitude of complications, including multi-organ impairment, partially due to the abundant expression of ACE2 in all human tissues.
.jpg)
SARS-CoV-2 virus binding to ACE2 receptors on a human cell, the initial stage of COVID-19 infection. Image Credit: Kateryna Kon / Shutterstock
However, a scientist from the University of Zaragoza and Agencia Aragonesa para la Investigacion Foundation in Spain sets to uncover an explanation as to why organ damage happens selectively rather than impacting the whole body.
Selective damage
What was first identified as another respiratory disease akin to the common flu has now taken the lives of more than 738,000 people and infected more than 20.19 million worldwide. The latest strain of the coronavirus, SARS-CoV-2, has been dubbed as an invisible enemy, and as the pandemic evolves, new symptoms continue to appear.
Aside from symptoms, as more people are infected with the virus, new information has been added to the potential complications linked to COVID-19. Some organs in the body are impacted by the virus, while others appear to be spared.
Published in the journal Chaos from AIP Publishing, the study explains why particular organs are affected by the viral infection while many other tissues contain ACE2 receptors, the gateway of SARS-CoV-2 into the human cell.
"This receptor is ubiquitous in most human organs, such that if the virus is circulating in the body, it can also enter into other organs and affect them. However, the virus affects some organs selectively and not all, as expected from these potential mechanisms," Ernesto Estrada, from the University of Zaragoza and Agencia Aragonesa para la Investigaciónm, explained.
Explaining why some organs are spared
When the virus enters a human cell, the proteins of the pathogen interact with those in the body, paving the way for its effects to be established. The coronavirus damages only some organs, while others are not affected at all.
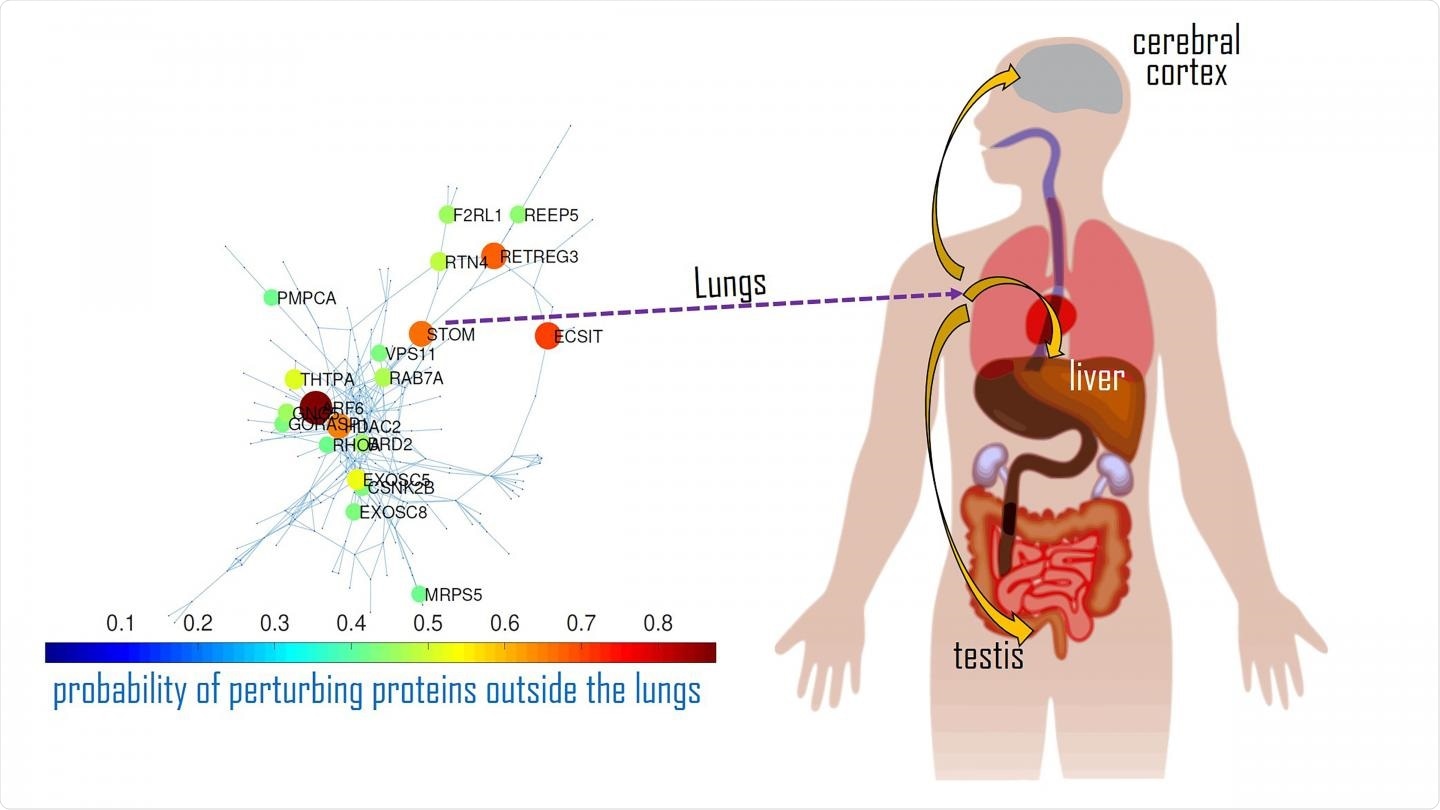
An interaction map of the main disease activators for SARS-CoV-2 in the lungs and how they impact proteins in other organs. Image Credit: Ernesto Estrada
Estrada believed there must be a different pathway for its transmission. To explain, he considered the displacements of proteins prevalent in the lungs and how they interact with proteins in other organs.
"We consider here diffusive processes through the protein-protein interaction (PPI) network of proteins targeted by SARS-CoV-2 as an alternative route. We found a subdiffusive regime that allows the propagation of virus perturbations through the PPI network at a significant rate," the researcher wrote in the paper.
"By following the main subdiffusive routes across the PPI network, we identify proteins mainly expressed in the heart, cerebral cortex, thymus, testis, lymph node, kidney, among others of the organs reported to be affected by COVID-19," he added.
Estrada clears that for two proteins to find each other and establish an interaction complex. They need to move inside the cell in a subdiffusive way, which is likened to a drunkard walking on a crowded street wherein the crowd gives challenges to the stunting displacement and making it harder for him to his destination.
Further, proteins in a cell are faced with many challenges they need to surpass to interact. Some of the proteins also exist within the same cell or organ, but others do not. Because of the complexity of these mechanisms, Estrada developed a mathematical model to allow 59 proteins within the lungs, which work as major activators that affect other human organs. This triggers a chain of interactions, starting with this set, stimulating changes in proteins along the way until eventually affecting their health.
"Targeting some of these proteins in the lungs with existing drugs will prevent the perturbation of the proteins expressed in organs other than the lungs, avoiding multi-organ failure, which, in many cases, conduces the death of the patient," Estrada explained.
Estrada also found that there are potential routes of propagation of the perturbations from proteins in the lungs, to proteins expressed in other tissues, including the heart, thymus, cerebral cortex, lymph node, prostate, testes, liver, duodenum, small intestine, kidney, among others that have been reported as damaged by COVID-19.
He noted that further studies are still needed to determine how the impacted proteins travel between organs.
Source:
Journal reference: