Great question. I am a pediatric infectious disease physician and have been in this field for 30 years. Pneumonia is an important infection that affects all ages of life, especially the very young and the elderly.
We have struggled with poor yield with the tests that we have had. There is the potential for development with new diagnostics that improve outcomes for individual patients. Furthermore, the unique thing about infectious diseases is that they affect others besides the individual patient because of the effect on the community from antibiotic use. Hence, an accurate diagnosis would improve outcomes for the community as well.
The issues we have had with diagnostics has been noticed by clinicians as well as by those who create guidelines for the care of these patients. I'm excited to have recently joined Karius because they are pushing the diagnostic envelope with a new blood test that allows us to increase the yield of making a diagnosis at the level of the actual microbe (or germ) that is making the patients sick.
I joined them because I was excited about their technology and the advances it would have for many patients, including those with pneumoia. The Karius Test has been on the market for over three years now and is helping patients on a daily basis by making a more accurate diagnosis.

Image Credit: Kateryna Kon/Shutterstock.com
How does pneumonia occur and what happens to the body? How common are pneumonia cases?
Pneumonia is very common. It is the most common cause of hospitalization and mortality in the Western world for infants and the second most common in the developing world. It also affects the elderly disproportionately, but we see it at all ages. It occurs through several different mechanisms depending on the microbe that is causing the pneumonia.
The most common types of pneumonia we see are microaspiration from microbes that colonize our nose and throats. In the right circumstance, they get into the lower airways, past the larynx (voice box) that protects those airways, and cause pneumonia, an infection in the lungs.
There are unique microbes that get into the lungs because they are dispersed in the right size particles - particles small enough to not be filtered by the nose and throat when you breathe in. They are breathed in straight to the lungs and can cause pneumonia.
Lastly, there is macroaspiration, where you choke on something like during emesis or eating. This allows microbes to get into the lung and also cause pneumonia. Those are the three main mechanisms that we see in people who acquire pneumonia.
Why does pneumonia often go undiagnosed?
As you can imagine, one of the more common causes is microaspiration. That microaspiration often occurs with organisms that are already in your nose and throat.
The nose and throat are colonized with different bacterial organisms. In order to make a diagnosis, we must get a specimen from the lower respiratory tract, from deep down in the lungs where pneumonia is causing the problem, but that requires that specimen to pass through the upper airway.
However, as that sample passes through the upper airway microbes there may contaminate the specimen. We have different techniques to help sort that out, but it remains problematic and difficult to be certain about what is happening in the lower airway because of that issue.
This can be especially difficult for patients pre-treated with antibiotics because you tend to pick up resistant microbes in the upper airway that may not have anything to do with what is going on in the lower airway. Those are some of the challenges we face.
As I mentioned, blood culture does not work very well. It is not very sensitive and only about 10 or 15% of blood cultures are positive and reflect what is happening in the lung.
Some rapid diagnostic tests have been developed for upper airway pathogens that cause pneumonia such as viruses. Those are very sensitive. However, they do not pick up some of the bacterial organisms that cause what we refer to as superinfection. Often an influenza virus, for example, will make you ill to start with, but then you will get a bacterial infection on top of it.
The influenza test in the upper airway can make the diagnosis of pneumonia, but there is not a good test to tell whether you have developed bacterial pneumonia on top of that or which microbe has caused the superinfection. That is another challenge that we face.
What are the issues with the current standard culture-based tests for pneumonia?
The blood culture test is frequently not positive. With the sputum culture, we face contamination from the upper airway, and the microbes that cause pneumonia frequently colonize (or, reside in) the upper airway. Some microbes are not readily detected because they are difficult to grow, and we have to use other types of tests to detect them.
In some situations, pneumonia leads to either pleural effusion or pus in an empyema that collects outside of the lung in the chest space. Sometimes patients have to have that material sampled for culture directly through the chest wall. Even when we do a very invasive procedure like that, we often do not get the microbe that is making the patient sick.
All of these problems have frustrated clinicians over the years. As you can imagine, we are talking about a lot of different tests and a lot of different test methods to try and diagnose a condition.
There is a big difference between a blood test and having a needle stuck in your chest, or having a tube put down your throat to take a specimen from within your lungs. Clearly, the blood test is the preferable option.
That is the exciting thing about the Karius Test—we can diagnose from a simple blood draw without doing any of these invasive procedures, without struggling with some of these things that hamper the traditional tests and make a diagnosis of over 1400 organisms.
Since I have come to work at Karius, I see daily how we are making unexpected diagnoses and changing patient therapies for the better. It has been really exciting.
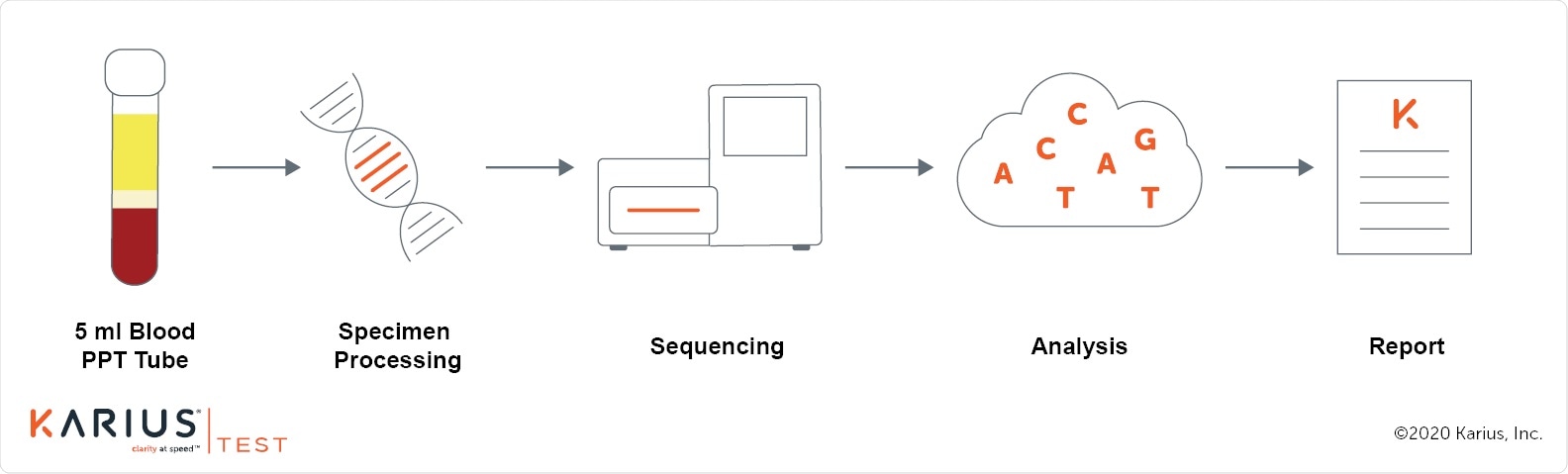
Image Credit: Karius
Why is advanced diagnostic testing for pneumonia better and how does it work?
The Karius Test looks for small pieces of the microbial DNA in the blood. As these organisms are fought and killed by our bodies, they release small pieces of DNA. The lungs are very vascular and have a rich blood supply because that is how they exchange oxygen and bring it to our bodies. The DNA from these organisms is readily released into the blood.
We enrich that blood to remove much of the human DNA (which is most of what is in the blood) and use advanced molecular techniques to sequence the microbial DNA and analyze it to identify which of those DNA pathogens are causing the infection.
Normally, we really struggle when somebody has received a dose of antibiotics before they come to the hospital because that decreases the yield on some of those tests that have been traditionally used. The exciting thing about this test is that those antibiotics are killing these organisms in addition to your body killing these organisms.
The Karius Test persists in a positive state longer than some of those traditional tests so we can make the diagnosis even in those difficult situations where somebody has already received a dose or two of treatment.
In fact, in a pediatric study that we published, using the whole gamut of traditional microbiology techniques, researchers were only able to make a diagnosis in about 45% of the cases in these critically ill patients. When they utilized the Karius Test, the diagnostic yield improved to almost 90%.
So, you can see what a tremendous difference it made for those patients with complicated pneumonia. In half of those patients, this led to an antibiotic change that was for the better - a more focused course of antibiotics with a lesser likelihood of side effects. None of those patients relapsed, showing that there was no problem with focusing the antibiotics more clearly for the organisms that we detected. That is very exciting information.
Brian's Story from Karius on Vimeo.
The CDC has reported a large increase in pneumonia deaths due to COVID-19. Why is pneumonia common in COVID-19 infections?
COVID-19 is one of those pathogens that has a predilection, like some of the other viral infections and like certain types of unusual bacteria, to bypass the upper respiratory tract and go to the lung. That is why we see pneumonia so commonly in COVID-19. It is the major reason for condition deterioration in COVID-19 leading to hospitalization and ICU care.
Could an improvement in the diagnosis of pneumonia benefit the treatment of COVID-19 patients and help to prevent deaths?
Indirectly, yes. There are a couple of things we struggle with regarding COVID-19. As you can imagine in the middle of a pandemic like this, where pneumonia is a big part of the serious presentation of the illness, at the moment when a patient presents with pneumonia at the hospital, the first thought in everybody's mind is, "Is this COVID-19?"
The current COVID-19 tests are not very sensitive. Up to a quarter of the time, there can be false negatives. People have sort of a one-track mind and we have seen patients who have had up to seven COVID tests because people just do not believe that they do not have COVID and do not think about the other potential causes of pneumonia.
We have seen great utility of our tests in that situation. People finally say, "Well, maybe we should look for something else." They send our tests, find something that is treatable, and the patient improves.
The other situation that we see is that some of these patients get very sick and end up on the ventilator in the ICU. That in itself leads to complications that we call superinfection. When you are very compromised on a ventilator, bypassing the normal protective mechanisms you have for your airway, a complication of being in the hospital is developing a hospital-acquired or ventilator-associated pneumonia. That is another place where we can offer help to these COVID patients and help diagnose bacterial and other causes of those superinfections.
Image Credit: Dotted Yeti/Shutterstock.com
Would an improvement in pneumonia diagnosis be beneficial in dealing with future pandemics?
Absolutely. Of course, at this point, it depends on the organism causing the pandemic. Our test is a DNA test that does not detect RNA viruses, but numerous DNA based pathogens could cause a future pandemic. DNA viruses, fungi, parasites, and bacteria could all be detected by our test.
One of the beautiful things about our test is that it is broad and open-ended. For many tests that we do to diagnose infections, you have to know what you are looking for and so they are not as appropriate for unusual, emerging infections. Our test does not require that. We sequenced all the microbial DNA that is present in the blood and could pick up a novel agent causing a pandemic.
Why do infectious diseases need better diagnosis practices in general?
First of all, a more accurate diagnosis leads to a more accurate choice of treatment for the individual patient, which improves outcomes and is very important. It also decreases side effects. Using very broad-spectrum antibiotics causes side effects. The most common is diarrhea, and that can lead to life-threatening intestinal problems that affect individual patients.
Our bodies are full of beneficial organisms that are affected by the antibiotics that are used to treat an invasive infection like pneumonia. Exposure to antibiotics affects those microbes as well and can lead to the development of resistance.
Once somebody has organisms in their body that have developed resistance, they can take them home to their families. Their families can then spread them to the community. One of the things we see in infectious diseases and have to deal with regularly is the evolution of the microbes that cause infection to become more and more resistant to antibiotics which makes it harder and harder for us to treat them.
Therefore, a more accurate diagnosis and focused treatment of the infection benefits not only the individual patient but also the community at large. It makes the development of resistance less likely and preserves our precious antibiotics which are becoming harder and harder to develop.

Image Credit: Joel bubble ben/Shutterstock.com
What steps are you taking to make advanced diagnostic testing a standard practice?
In the same way that we have to be judicious with our use of antibiotics for patients, we also have to deploy a diagnostic test at the right point in the course of determining what is the best way to treat that patient. Several things are needed to make that happen.
One of them is for us to work with the infectious disease society of America, the American thoracic society, and the other guideline-generating bodies around the world to make them aware of the benefit of the test - the fact that it detects over 1400 pathogens from a single blood draw and provides an answer typically within 24 hours of receipt at the laboratory.
We can help determine within their guidelines when the best time to deploy that test is for the population, to inform physicians about the best way and time to use it. These guidelines often drive physician behavior concerning how they diagnose and treat important and severe conditions like pneumonia.
What are the next steps for your research into pneumonia and advanced diagnostic testing?
We would like to continue to learn which populations of patients benefit most from this test.
Currently, we have a study in progress at 6 centers in the U.S. (which is still recruiting for additional centers) looking at the use of this test for immunocompromised patients. These patients are compromised because they have because they are receiving treatment for cancer with medications that suppress their immune system.
This means that they are at risk for the usual causes of pneumonia as well as more unusual causes of pneumonia that are even more difficult to diagnose. This ongoing study is designed to evaluate how this test can help with the management of those patients.
Those are patients that are even more likely to have invasive tests done to try and make that diagnosis because they are at a much higher risk of complications and getting these unusual organisms. Hence it is important to see if our tests can help prevent invasive procedures in some of those patients. I think that is exciting and we are excited to see the results of that study.
Where can readers find more information?
Community-acquired Pneumonia in Children: Cell-Free Plasma Sequencing for Diagnosis and Management
Secondary Infections in COVID-19 and their Impact on Disease Severity
https://kariusdx.com/
Evaluation of Plasma Microbial Cell-Free DNA Sequencing to Predict Bloodstream Infection in Pediatric Patients With Relapsed or Refractory Cancer
About Dr. William La Via
Dr. La Via is a Medical Director for Karius. He completed pediatric residency training as well as pediatric infectious disease fellowship training at the UC Irvine Medical Center. 
After training, he has spent 14 years in practice, mostly in academic infectious diseases and 3 years in private practice.
He subsequently worked in Medical Affairs at MedImmune, a specialty division of AstraZeneca, for 11 years supporting their portfolio in infectious disease biologics, vaccines, and respiratory biologics.