Once we started hearing of pneumonia and the need to put patients on a ventilator, that was a pretty big clue that we are dealing with lung injury and development into ARDS.
What is acute respiratory distress syndrome (ARDS)?
ARDS is a rapidly progressing inflammatory disease characterized by the disruption in the endothelium (blood vessel wall) and epithelium barrier, which leads fluids and white blood cells, typically neutrophils, to enter into the lung airspace.
The fluid in the lungs compromises gas exchange – leading to difficulty breathing, with the excess white blood cells increasing inflammation. The end result is lung failure and death.
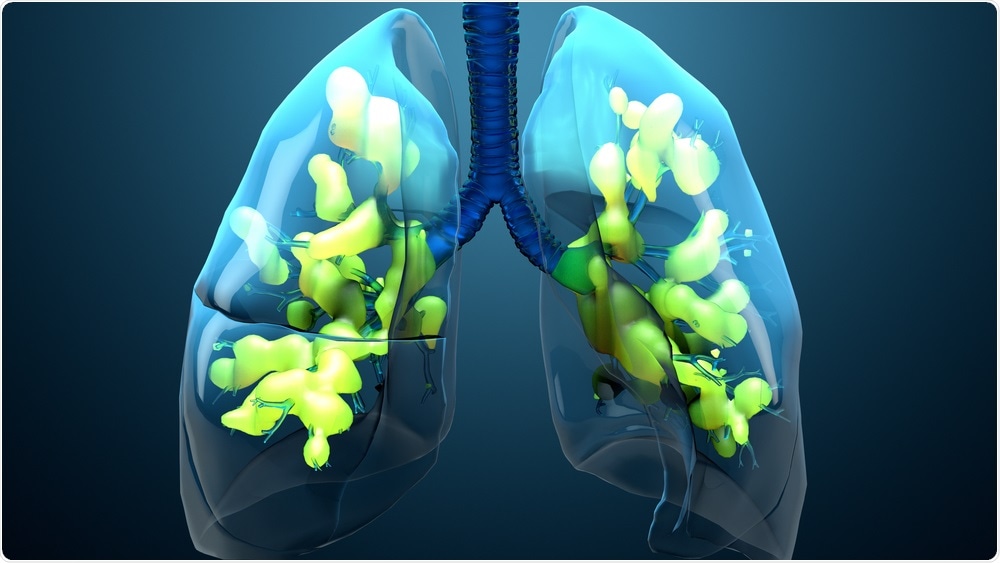
Image Credit: Design_Cells/Shutterstock.com
What are neutrophils, and what is their role within the immune system?
Neutrophils are the body’s first responder. Their job is to mobilize to a site of infection or injury with the primary goal of fixing the problem, by either eating the pathogen (e.g., phagocytosis) or secretion of potent chemicals that kill the pathogen.
Neutrophils are not specialized white blood cells. Why is this sometimes a problem?
A non-specific response means the action if extended longer than needed, can begin to cause harm. It is very much like throwing a bomb over the fence – you will kill the invader, and soon enough anything else that is close by.
Image Credit: Kateryna Kon/Shutterstock.com
What role do neutrophils play in COVID-19 infections?
As the injury caused by the SARS-CoV-2 virus continues to propagate in the lungs, the lungs cells increasingly produce cytokines (danger signals) that call in the neutrophils and more monocytes.
This process of the cells going to the lungs in an extended period, creates a barrier rupture, aka lung injury which later develops into ARDS.
Again, once the neutrophils get into the lungs, they essentially edge on the resident immune cells (macrophages) in the lung, amplifying the problem, i.e., the inflammation.
How did you carry out your research into neutrophils and ARDS?
We used human blood to evaluate the response of white blood cells, including neutrophils, to the release of cytokines from the lungs during viral infection.
We are next working with animal models, mostly mice, in which we can recreate the human version of the lung injury.
What did you discover?
Professional phagocytes, e.g., macrophages and dendritic cells, prefer sphere-shaped particles, whereas neutrophils prefer rod-shaped particles. Why do different white blood cells have varying preferences for different shapes? The simple answer is evolution.
The primary role that neutrophils have in the body is to clear out bacteria. Many of the common bacteria are rod-shaped, so evolutionarily speaking, the neutrophils have perfected the act of eating rods in the way the other phagocytes have not had to.
Do you believe that this research can help to reduce the number of people dying from COVID-19?
Yes, if we can make these rods in the right size and shape, using materials that the body can tolerate, i.e., biocompatible and degradable, then we can use the particles to bring drugs directly to the cells to quiet them down.
.jpg)
Image Credit: Andrii Vodolazhskyi/Shutterstock.com
What are the next steps that need to be taken before your research can be carried out in clinical trials?
We would need a biocompatible material and to identify the right drug to target. These will then need to be tested in an animal model before being able to get in the clinics.
We are working with a new start-up company, Asalyxa Bio, Inc., to bring one such formulation to the clinic for COVID19 rapidly.
Where can readers find more information?
https://advances.sciencemag.org/content/6/24/eaba1474
About Professor Lola Eniola-Adefeso
Professor Lola Eniola-Adefeso is the University Diversity and Social Transformation Professor of Chemical Engineering and Biomedical Engineering at the University of Michigan.
She has 20+ years’ research experience in neutrophil mechanisms in acute and chronic inflammatory diseases and is an expert on vascular-targeted nano/microparticle technologies for disease treatment.
She is a Fellow of the American Institute of Medical and Biological Engineering (AIMBE). She is serving as CTO of Asalyxa, a recently launched start-up company, to develop particle technology for combating neutrophilic injury.