A new study by researchers at Strasbourg University Hospital and published on the preprint server medRxiv* in June 2020 shows that COVID-19 antibody responses may sometimes be lacking following exposure to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This could lead to a significant underestimation of the number of infections and the number of individuals who have achieved immunity.
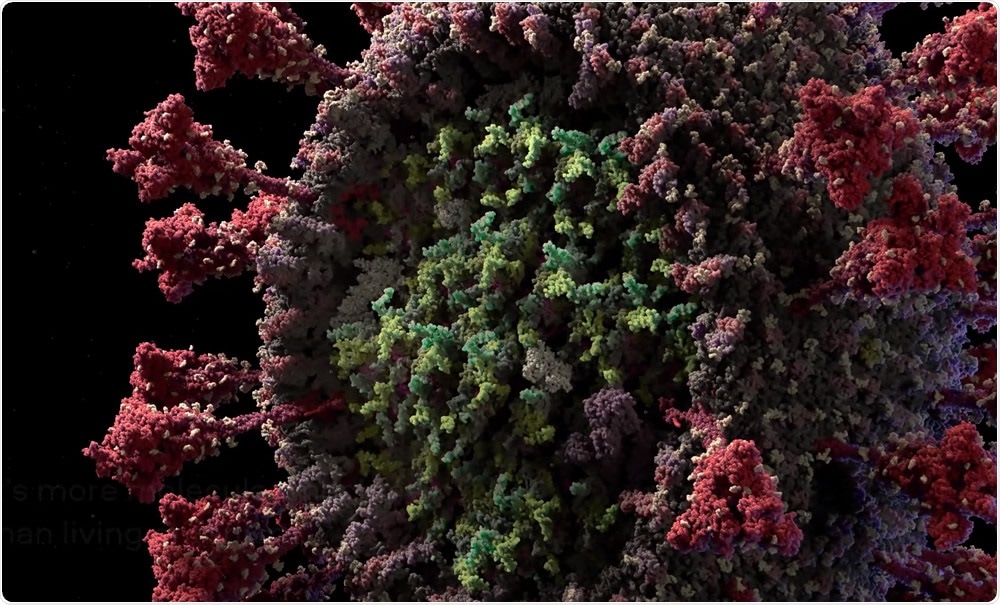
3D model of the SARS-CoV-2 virus at atomic resolution. Image Credit: Visual Science
Even as COVID-19 cases continue to rise all over the world, scientists are working to discover the true incidence and prevalence of infection. The most common method to find the number of infections at any given point is a combination of viral RNA detection by reverse transcriptase-polymerase chain reaction (RT-PCR) testing, and of prior or current infection by antibody testing, or serology.
The ability to detect immunizing infections is essential in predicting the speed of return to economic activity in a public workplace. Serologic tests aim at finding neutralizing antibodies to SARS-CoV-2, and the US, as well as some EU countries, is considering the possibility of issuing immunity certificates based on these tests.
However, a potential source of error was uncovered when several household members of COVID-19 patients tested negative for antibodies by these tests, despite undoubted exposure to the index case. Some other viruses have also been associated with the same phenomenon. In such cases, specific T cell responses have been demonstrated, which prove that infection has occurred and been successfully overcome.
The Study: Antibody vs. T Cell Response
The current study aimed at describing T cell and antibody responses in seven families who showed this pattern. Each family had at least one confirmed case (by RT-PCR) and at least one contact whose antibody test was negative. All index cases were recovered mild COVID-19 patients with infection history between March 2 and March 25, 2020. The serologic tests were carried out between May 7 and May 28, 2020.
A control group of 10 healthy non-exposed donors, also seronegative for SARS-CoV-2, was also set up. Three assays were used for antibody detection, with high sensitivity and specificity. The RT-PCR assay was capable of detecting as few as 10 copies/reaction.
The T cell response was detected via an interferon-gamma (IFN-γ) ELISpot assay on fresh peripheral blood mononuclear cells (PBMCs).
All nine index cases (recovered) were positive for antibodies. Also, they had specific IFN-γ responses against four to eight viral antigens, always including S1, S2, N, and M proteins, at 47-69 days from the earliest symptom. This suggests that antiviral T responses persist in recovered mild infection for at least this duration.
Of the eight seronegative family contacts, six showed specific T cell responses to one or more of the viral antigens. All patients and contacts, and 9/10 healthy donors, showed a high frequency of specific T cell responses to human coronavirus strains HCoV 229E or HCoV OC43.
Patterns of T Cell Response
The pattern of response to viral antigens differed from index patients to contacts. The immunodominant antigens in patients were the viral structural proteins S1, S2, M, and N, and these produced T cell responses in every index patient. The accessory proteins of the virus also elicited T cell responses in a significant proportion of these patients. The researchers say, “For the first time, our data demonstrate that the mild forms of COVID-19 induce a significant T cell response detectable at least 69 days after symptom onset.”
Symptoms developed in five of six contacts who showed specific T cell responses. Most of these individuals reacted to one or two structural or non-structural proteins, but the T cells producing IFN-γ against the virus belonged to the same classes seen in the index patients. This could indicate the presence of specific anti-SARS-CoV-2 T cell immunity.
Cross-Reaction or Subclinical Exposure?
A recent study found that anti-S T cell responses were found in 40% to 60% of individuals unexposed to the SARS-CoV-2, suggesting the presence of cross-reactive T cell immunity to other coronaviruses. This is confirmed by the fact that in the current study, the magnitude of the T cell responses, both CD4 and CD8 cells, against common coronaviruses HCoV 229E and HCoV OC43 showed no significant differences between index patients, contacts and unexposed healthy donors.
The difference was evident concerning specific anti-SARS-CoV-2 IFN-γ-producing T cells, which were present at significantly higher levels in index patients and their contacts. This means the presence of specific T cell responses against the virus, rather than only cross-reactive antibodies.
Implications and Future Applications
This study is the first to show that family contacts can show specific T cells response to SARS-CoV-2 without a detectable serological response. The presence of the T cell response proves that this may be a more sensitive detector of exposure to the virus than the humoral tests and that the patient developed a transient or limited infection in the past.
The presence of a detectable T cell response, specifically targeting SARS-CoV-2 could be the result of the subclinical transmission of the virus. This could happen because of the short-lived bouts of viral replication because of exposure to low doses of the virus. Alternatively, it could reflect the activation of innate protective immunity or incompetent replication due to defects in the viral genome.
The question remains as to the nature of these T cell responses: do they confer protection against repeated infection? Nonetheless, the results of this study help understand more of the virus’s natural history, indicate the possible underestimation of viral exposures in the population, and could help in tracing future viral spread and in vaccine development.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Gallais, F. et al. (2020). Intrafamilial Exposure to SARS-CoV-2 Induces Cellular Immune Response without Seroconversion. medRxiv preprint. doi: https://doi.org/10.1101/2020.06.21.20132449. http://medrxiv.org/cgi/content/short/2020.06.21.20132449
- Peer reviewed and published scientific report.
Gallais, Floriane, Aurélie Velay, Charlotte Nazon, Marie-Josée Wendling, Marialuisa Partisani, Jean Sibilia, Sophie Candon, and Samira Fafi-Kremer. 2020. “Intrafamilial Exposure to SARS-CoV-2 Associated with Cellular Immune Response without Seroconversion, France.” Emerging Infectious Diseases 27 (1). https://doi.org/10.3201/eid2701.203611. https://wwwnc.cdc.gov/eid/article/27/1/20-3611_article.