The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a new human pathogen, and as such, there is no pre-existing immunity to this virus. As a result, the virus has rapidly spread among the world’s population, causing different degrees of COVID-19, from asymptomatic to fatal disease. The current study is aimed at understanding how individual immune responses contribute to the clinical severity of the condition.
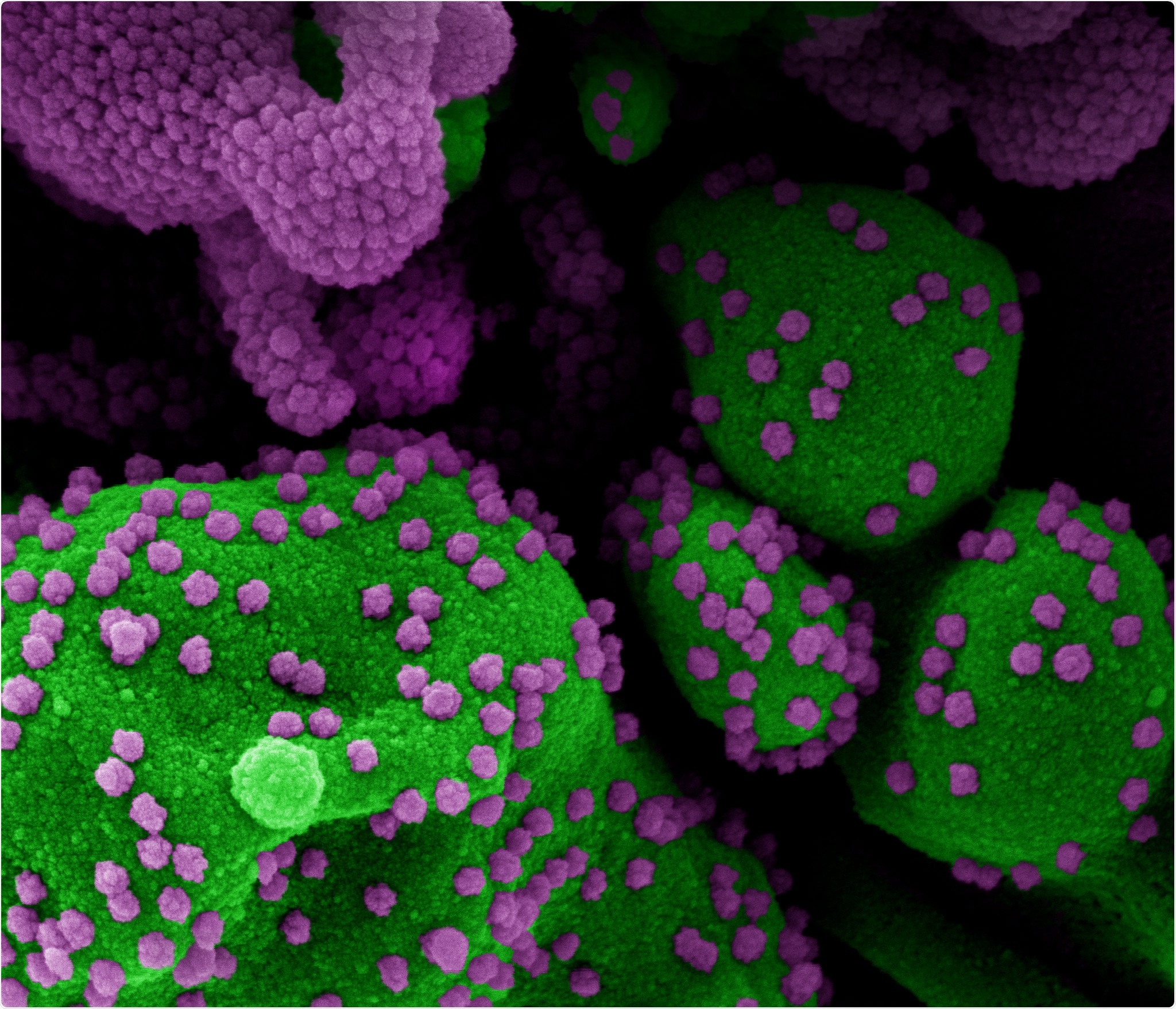
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of an apoptotic cell (green) heavily infected with SARS-COV-2 virus particles (purple), isolated from a patient sample. Image at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Cellular immunity in COVID-19
COVID-19 causes a drop in lymphocyte count, varying with disease severity, and reflected in both CD4 and CD8 T cell counts. The few T cells that are found in severe disease are functionally exhausted, and the lower the count, the worse the outcome predicted. Healthy individuals who have not been exposed to the virus still show cross-reactive T cell responses due to other coronavirus infections. Still, specifically reactive T cell clones are found at higher levels in COVID-19 convalescents.
Humoral Immunity in COVID-19
Anti-SARS-CoV-2 antibodies occur at high levels in severely ill COVID-19 patients and are seen first after 2-3 weeks from the first symptoms. Neutralizing antibodies are produced and help to eliminate the virus, as seen by the role played by convalescent plasma in the recovery of severely sick COVID-19 patients. These antibodies target the receptor-binding domain on the S1 subunit of the spike protein.
As expected, first to arrive on the scene are the Immunoglobulin M (IgM) type, followed by Immunoglobulin G (IgG) antibodies. Earlier studies show that Immunoglobulin A (IgA) may also be produced against the virus in a robust and prolonged manner. However, patients with high antibody levels still develop severe disease, which may suggest that these, by themselves, cause antibody-dependent enhancement (ADE) of viral infection and injury, or at best, are ineffective.
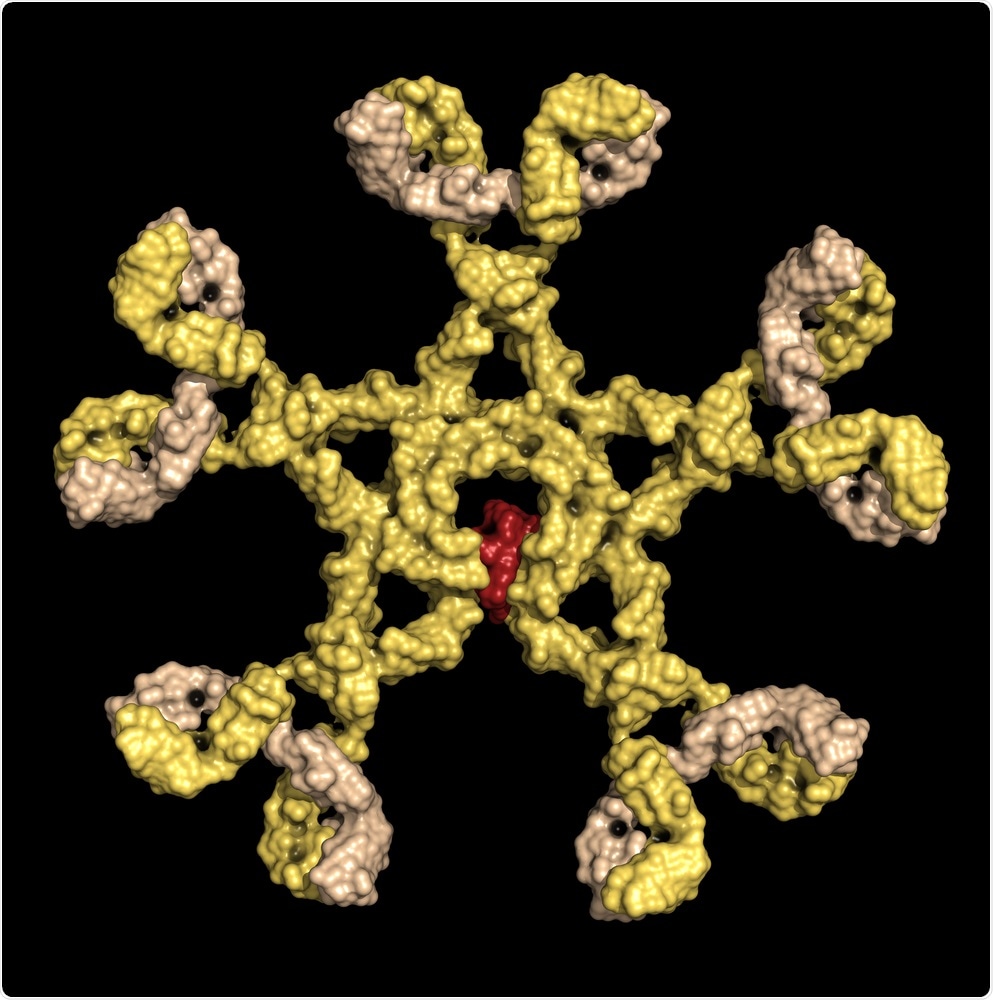
Immunoglobulin M (pentameric IgM). IgM are the first antibodies to appear during an infection. Detection of IgM is often used in the diagnosis of infectious disease. Surface representation. Image Credit: StudioMolekuul / Shutterstock
The current study measured both antibody levels and T cell counts in mild, severe, and asymptomatic COVID-19 patients, as well as their healthy contacts. Clinically, severely ill patients had a median age of 65 vs. 55 for mild disease. There was no skewing of the sex ratio. Asymptomatic patients had a mean age of 40, and the sex ratio was 4:1 in favor of females. The healthy contacts had a mean age of 41 years and a sex ratio of approximately 1:2 in favor of females.
Monocytes and Natural Killer Cells
The researchers found that neutrophils and monocytes dominated peripheral blood mononuclear cells (PBMCs) with lymphopenia in severe illness. However, normal T cell frequencies are seen in mild and asymptomatic disease.
When only T cells were excluded from the analysis, they found a fall in the natural killer (NK) cells and an increase in monocyte count in severe and mild disease alike. The persistence of this pattern over time and across all patients groups appears to indicate that this is a characteristic of the disease and not a result of testing at some specific point of the disease. They tested the validity of this observation in 77 patients who had severe disease and found that non-ICU cases had significantly more NK cells than ICU patients. Moreover, NK cell counts went up in recovered severe disease but remained low in others until they died. Perforin expression on NK cells in ICU patients was also lower.
Based on the expression of CD16, monocytes with the CD14 marker can be differentiated into three types as they mature and display different functionalities. The earliest type, or classical monocytes, are important in anti-pathogenic and anti-inflammatory responses. Intermediate monocytes develop from the former type, have Toll-like receptors (TLR) which, when stimulated, trigger inflammatory cytokine release and show clonal expansion in severe infections. The third type is nonclassical monocytes, which help resolve inflammation and keep blood vessels healthy. Nonclassical monocytes are reduced in number in severe COVID-19 compared to asymptomatic or mild disease. Intermediate monocytes show an increasing trend.
Thus, a monocyte-to-natural killer ratio (MNKR) is above 1 in mild infection but higher in severe COVID-19, indicating a balance between the two cell types is needed to overcome the infection. Predominant NK cells are found in asymptomatic and monocytes in severe infection.
In severe disease, monocytes increase in number, secrete inflammatory cytokines, and may cause a cytokine storm, especially when monocytes recruited to the lung enhance the inflammatory response still further. Thus therapies that increase natural immunity but counteract excessive proinflammatory cytokine release can help contain severe COVID-19.
T and B Cells: Adaptive Immunity
The T cell pool remained unchanged, on the whole, in asymptomatic people, but with COVID-19 infection, CD4 cells showed HLA-DR expression. In contrast, CD8 T cells were activated only in severe disease and were linked to an increase in the number of effector memory cells with high cytotoxicity and of exhausted terminally differentiated memory T cells.
Total B cells were reduced, while plasmablasts were increased in severe disease. B cells produce antibodies either as plasmablasts in circulation or as plasma cells in various tissues. TLR can stimulate memory B cells and rapidly induce the production of antibodies independent of T cell or germinal center stimulation.
IgA levels are high in asymptomatic patients in early disease, but is undetectable in 5-7 weeks. IgG is mostly low. However, both IgA and IgG are late to rise, and both remain low in mild disease, but rising in severe disease. In other words, only a long and severe infection with SARS-CoV-2 induces neutralizing antibodies.
IgA, Bats and Asymptomatic Infection
The high IgA in the former situation may rapidly neutralize the virus in the respiratory mucous membrane and so prevent a complete adaptive immune response. The researchers suggest that perhaps this may be due to the early activation of pre-existing innate or natural IgM antibodies, or cross-reactive antibodies, from memory B cells that quickly undergo a class switch to IgA instead. However, if this early rise in IgA is lacking, the virus can survive longer and induce germinal center differentiation in the local lymph nodes.
Thus, asymptomatic COVID-19 might be like bat coronavirus infection, controlled by NK cells and natural antibodies. In severe disease, the adaptive immune response is more robust and more diffuse. Only more research can tell if and how long specific memory persists in patients with mild or asymptomatic disease.
Implications
The public health implications of this study are tremendous. Natural infection cannot build up herd immunity because it does not activate an adaptive immune response. As a result, they say, “Social distancing and infection control will remain indispensable to limit the spread of SARS-CoV-2 until effective vaccines able to induce strong and long-lasting B- and T-cell memory are available.”
At the same time, current IgG-dependent serologic screening may not be useful because of the rapid fall in IgG levels to undetectable levels in mild cases, and the IgA production in asymptomatic infection may lead to these being missed in screening. The result is a large underestimation of actual infections.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Carsetti, R. et al. (2020). Spectrum of innate and adaptive immune response to SARS-CoV-2 infection across asymptomatic, mild and severe cases – a longitudinal cohort study. medRxiv preprint doi: https://doi.org/10.1101/2020.06.22.20137141. https://www.medrxiv.org/content/10.1101/2020.06.22.20137141v1
- Peer reviewed and published scientific report.
Carsetti, Rita, Salvatore Zaffina, Eva Piano Mortari, Sara Terreri, Francesco Corrente, Claudia Capponi, Patrizia Palomba, et al. 2020. “Different Innate and Adaptive Immune Responses to SARS-CoV-2 Infection of Asymptomatic, Mild, and Severe Cases.” Frontiers in Immunology 11 (December). https://doi.org/10.3389/fimmu.2020.610300. https://www.frontiersin.org/articles/10.3389/fimmu.2020.610300.