The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has set off a worldwide wave of infections and death, with over 9.4 million cases and over 482,000 deaths to date. With few pharmacological tools to counter the infection, governments have resorted to mandating social distancing and shelter-in-place policies to restrict viral spread.
The Lockdown Toll
With physical isolation being necessary at the level of whole populations, the strain has been borne by economies, but also by individuals who are forced to change their behavior patterns overnight and sometimes avoid social interaction altogether. Moreover, the focus on handling and mitigating current and future COVID-19 waves may have resulted in less care for other illnesses, including obesity and type 2 diabetes.
Among the population groups at high risk for COVID-19, those with obesity, cardiovascular disease, and type 2 diabetes are known to be prone to more severe disease. This favors the public health policy of physical mobility restriction to protect these groups against the infection. However, as a result of these measures, the incidence of obesity may increase due to inadequate physical activity, strengthening of depressive tendencies, and lack of social interactions that support group exercise.
This could actually increase the number of those at higher risk of severe COVID-19, not including the other risks associated with obesity like chronic obstructive pulmonary disease, diabetes, and cardiovascular disease.
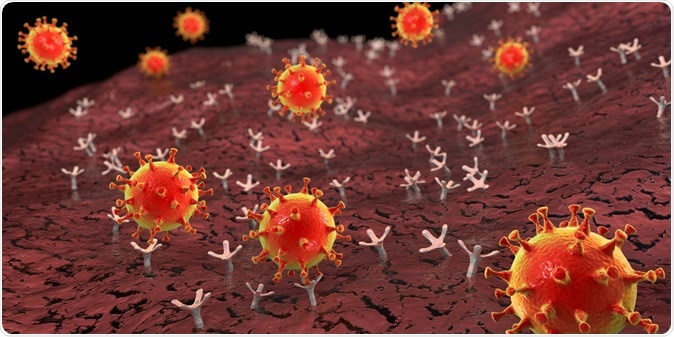
SARS-CoV-2 viruses binding to ACE-2 receptors on a human cell. Image Credit: Kateryna Kon / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The Study: Obesity Risk, Mortality, Associated COVID-19 Risk
The current study aims at measuring baseline mortality in severely obese individuals in England, the excess mortality in this group, and the effect of a higher body mass index (BMI) and physical activity on the incidence of and death from common risk conditions for COVID-19.
The study included almost 2 million individuals registered with their local health providers using electronic health records. The researchers found that severe obesity was not an indicator of high baseline risk of mortality unless there were two or more underlying illnesses.
They also discovered that the number of excess deaths directly due to severe COVID-19 in severe obesity, or due to other illnesses for which health services were affected by the pandemic, was not significantly increased. With a 10% infection rate, anywhere between 240 to 479 excess deaths might occur directly as a result of COVID-19, and 383 to 767 excess deaths as an indirect result.
However, they also found that as a result of a three-month lockdown, many more people could become obese, from almost 98,000 to 434,000, putting them at high risk for future disease. As expected, regular physical exercise could protect against this excess mortality during lockdown.
Obesity has been increasing in prevalence all over the world, and severe obesity is linked to a twofold risk of diabetes and a tenfold risk of cardiovascular death compared to the non-obese. However, both baseline and excess mortality due to COVID-19 in this group will occur in people who also have two or more other medical conditions. Thus, these other illnesses must receive due care, preventive strategies, early diagnosis, and diligent management to alleviate this risk of death.
This observation is important in the light of the fact that dealing with a pandemic may push aside healthcare measures for other chronic and less urgent conditions. This should be avoided by especially assigning a higher priority for these interventions.
How Does Obesity Increase the Risk of Poor Outcomes In COVID-19?
Obesity can increase COVID-19-associated risk in three ways, namely, by making the individual more vulnerable to the virus via altered immune responses; because of associated chronic illnesses that boost the risk, such as cardiovascular disease and chronic obstructive pulmonary disease, and finally, because the virus may act differently in obese individuals. Thus, rather than obesity, the target of health interventions should be the chronic diseases often associated with it, which are the determinants of the excess deaths.
Worldwide, it is seen that almost 4 million deaths are linked to a high BMI, about 40% in people who are not obese, and over 66% caused by cardiovascular disease. The pandemic is thus affecting the uninfected populations as well. Earlier studies have shown that diabetes figures could well rise in India, and childhood obesity in Italy, which will result in many more future deaths directly attributable to COVID-19, as well as indirectly caused by BMI-dependent cardiometabolic conditions.
The lockdown in the UK and other EU nations has seen a drastic increase in the time spent at home, a steep downturn in the longest distance traveled from home, a reduction in the steps walked, and thus physical activity. Scientists have suggested that exercise and other lifestyle modifications are equally important when it comes to reducing the risk of acquiring the infection as social distancing and physical isolation.
The current study recommends adding exercise to lockdown advice, but also analyzing the effect of lockdown on exercise while shaping lockdown policies. Though this is an observational study, it indicates that the “burden of chronic diseases, even with a 3-month lockdown, may lead to a greater burden of excess deaths, highlighting avoidance of BMI gain and physical activity as public health priorities during the pandemic.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources