With the continuing spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) even in places where the peak was thought to have passed, the search to find all routes of transmission assumes ever-growing urgency. Now, a new study published on the preprint server medRxiv* in June 2020 reports that viral RNA has been found to occur in HVAC (Heating, Ventilation, and AC) units in healthcare facilities. However, it is not clear if this represents a possible mechanism of viral transmission.
Earlier, hospital rooms have been found to harbor the viral RNA in the air, in the form of aerosols, which indicates that it could also be present in HVAC systems in these places. Even though the use of mechanical filters and room air exchangers is high in these centers to moderate or prevent the transmission of disease, the evidence is piling up that this may not be sufficient for the latter purpose in the case of SARS-CoV-2.
The SARS-CoV-2 virus has been found to persist for hours or days in the air and on some surfaces, respectively. This has led to increased emphasis on the cleaning of hands and surfaces, social distancing, face masks, and surveillance. However, such practices may fail to keep viral transmission low once lockdown relaxation begins, as people again come together for more extended periods, especially in rooms with HVAC service. The current study aims to understand how these services can contribute to the potential viral spread. In this way, modifications of HVAC guidelines can be implemented.
The Study: Detecting Viral RNA in Air Unit Samples

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
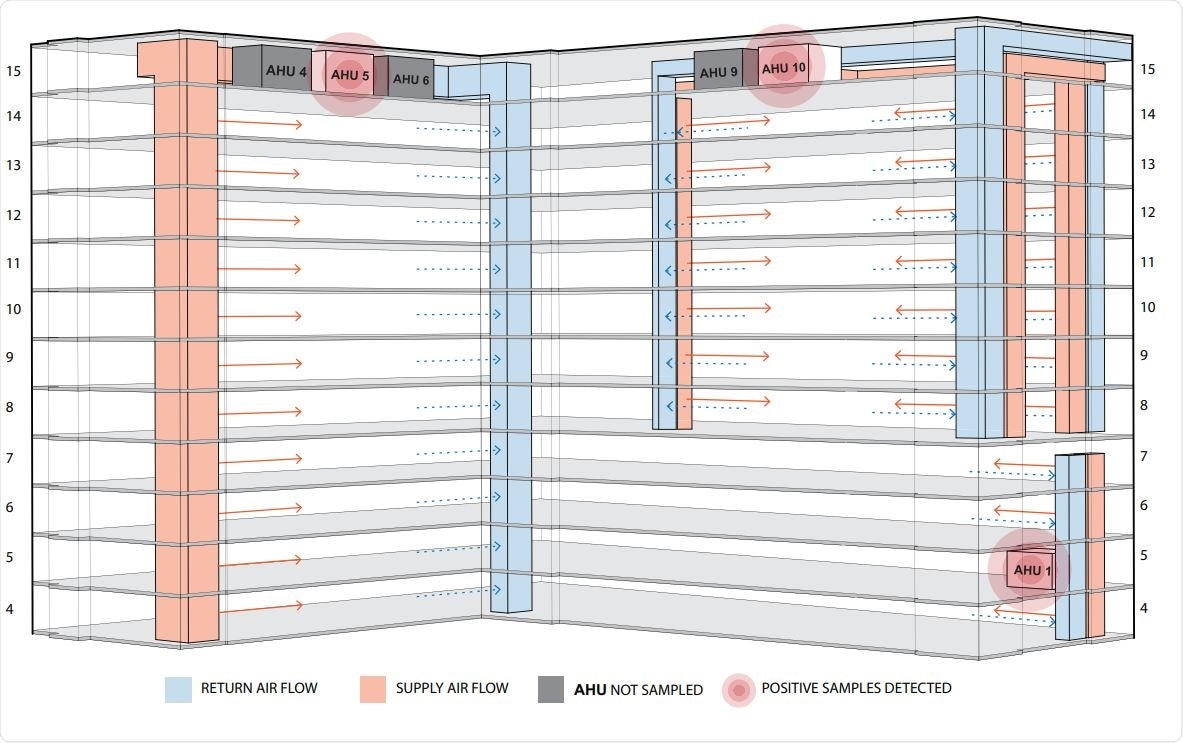
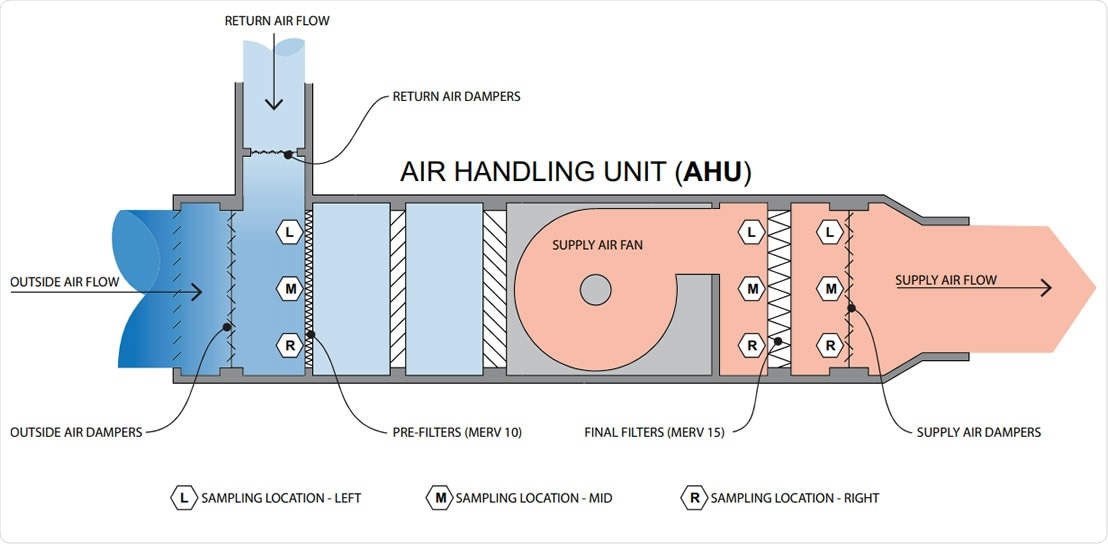
The researchers collected 56 samples from three different air handling units (AHUs) and found that viral RNA was present in about a quarter of them. About 35% of prefilter samples, 17% of final filter samples, and 21% of air damper samples contained viral RNA at detectable levels.
The most abundant number, with over 245 copies of the viral genes, was in the prefilters since this is where the outside air mixes with the recirculated building air. Conversely, the least abundance was at the final filter.
The researchers suggest that their results show the SARS-CoV-2 virus could be present at many locations along the mechanical AHUs, especially those which filter the air at multiple floors of a hospital unit housing COVID-19 patients. The virus was detectable for at least a third of the time at the air damper, which is the last sampling location.
At this spot, the recirculated air from inside the building is mixed with fresh air from outside, after it is passed through the prefilter and the final filter. In short, the use of modern filtration practices at the highest level of purification in a healthcare environment is still not sufficient to rule out the passage of the viral RNA and possibly viral particles through the HVAC systems, and therefore their re-entry into the hospital rooms.
While the researchers admit that this does not mean that patients are exposed to a risk of COVID-19 infection, it does show the possibility that the air from spaces housing infected patients could reach other spaces in the building containing other occupants, while containing the virus despite having been refreshed with 70% to 80% fresh air from outside.
Lack of Guidance on Aerosolized Virus
The researchers did not attempt to assess the infectivity of the samples. Still, earlier studies have shown that virus particles can be carried in an aerosol from the source by the air currents formed by HVAC systems. Even though the aerosolized virus is among the potential routes of airborne viral transmission, official health organizations such as the World Health Organizations or the Centers for Disease Control (CDC) have not provided guidelines on this transmission mechanism.
However, the buildings studied in the current research had HVAC, which exceeded the standards of the American Society of Heating Refrigerating and Air-Conditioning Engineers (ASHRAE) Standard 170-2017 Ventilation for Healthcare Facilities guidelines.
The use of negative pressure rooms for housing patients with COVID-19 significantly reduces the risk of such recirculation within HVAC systems. However, this type of room may not be found in sufficient numbers in the majority of hospitals and clinics to handle the current pandemic. Another factor to consider is the high number of individuals without symptoms or who are presymptomatic but are shedding the aerosolized virus in common air spaces.
In fact, the risk could be even higher in other buildings where such high-efficiency AHUs are not in place, as well as when HVAC systems take in less air from outside due to very cold weather.
Reducing the Risk
In such a situation, where aerosolized virus particles can be potentially passed on through recirculated air, the use of personal protective equipment (PPE) as per protocol, careful hand hygiene, keeping high touch surfaces disinfected, and the use of irradiation to eliminate viral particles should also be emphasized. The filters used should be of the highest possible efficiency and the design optimal to ensure relative humidity between 40% to 60%, while increasing the amount of introduced outdoor air.
Despite the limitations of the study, the researchers sum up: “The findings suggest the potential for HVAC systems to facilitate transmission by environmental contamination via shared air volumes with locations remote from areas where infected persons reside.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Horve, P. F. et al. (2020). Identification of SARS-CoV-2 RNA in Healthcare Heating, Ventilation, and Air Conditioning Units. medRxiv preprint. doi: https://doi.org/10.1101/2020.06.26.20141085. https://www.medrxiv.org/content/10.1101/2020.06.26.20141085v1
- Peer reviewed and published scientific report.
Horve, Patrick F., Leslie G. Dietz, Mark Fretz, David A. Constant, Andrew Wilkes, John M. Townes, Robert G. Martindale, William B. Messer, and Kevin G. Van Den Wymelenberg. 2021. “Identification of SARS‐CoV‐2 RNA in Healthcare Heating, Ventilation, and Air Conditioning Units.” Indoor Air, June, 10.1111/ina.12898. https://doi.org/10.1111/ina.12898. https://onlinelibrary.wiley.com/doi/10.1111/ina.12898.