Globally, more than 10 million people have been infected with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Of these, at least 5.39 million have recovered, but the question of long-lasting immunity and protection from being infected again remains unclear.
Now, a team of researchers at the Karolinska Institutet and Karolinska University Hospital in Sweden has found that the number of people immune to COVID-10 may be higher than previously thought, and that antibody testing may no longer be the appropriate tool to trace it.
The study findings are published on the pre-print server, bioRxiv*, and are not yet peer-reviewed.
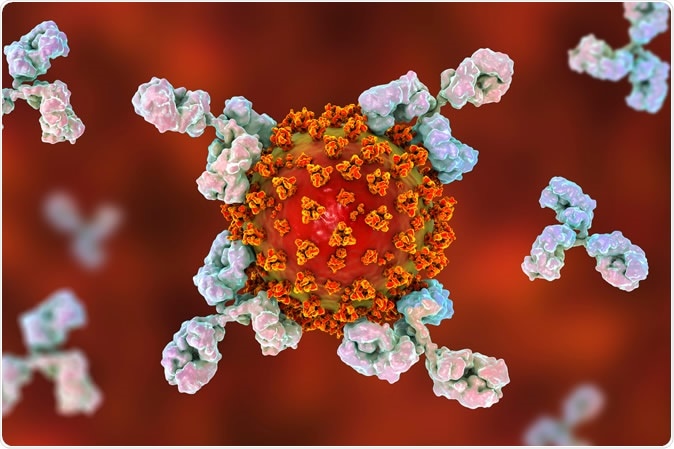
Antibodies attacking SARS-CoV-2 virus, the conceptual 3D illustration. Image Credit: Kateryna Kon / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
T-cell mediated immunity
Public immunity to the novel coronavirus, which causes the coronavirus disease (COVID-19), could be higher than antibody tests suggest. This also means that people who have not tested positive for antibodies can still show a T-cell mediated immunity to the coronavirus.
"T cells are a type of white blood cells that are specialized in recognizing virus-infected cells, and are an essential part of the immune system," Marcus Buggert, assistant professor at the Center for Infectious Medicine, Karolinska Institutet, and study lead author, said.
"Advanced analyses have now enabled us to map in detail the T-cell response during and after a COVID-19 infection. Our results indicate that roughly twice as many people have developed T-cell immunity compared with those who we can detect antibodies in," he added.
To arrive at their findings, the team conducted immunological analyses of samples from more than 200 individuals, a majority of whom had only mild or no symptoms of the viral infection. They included some patients admitted to the Karolinska University Hospital. Those who donated blood during the 2020 and 2019 periods were also included as the control group.
The team observed that those who had a positive COVID-19 test are not just the ones who showed T-cell immunity but also their exposed family members who were asymptomatic (had no symptoms). Further, about 30 percent of blood donors who donated blood in May 2020 had COVID-19 specific T cells, showing that the rate is way higher than previous antibody tests have shown.
However, it is unclear what level of immunity is provided by a T-cell response, although antibodies are believed to last only between three and six months.
The T-cell response was consistent with the measurements taken after immunization with approved vaccines for other viruses. Patients who experienced more severe COVID-19 created a robust T-cell response and an antibody response. Meanwhile, though some patients only had mild symptoms, there are times an antibody response could not be detected, but they may still show a significant T-cell response.
People may have established an antibody response, but either it had faded or was not detectable in tests.
"Our collective dataset shows that SARS-CoV-2 elicits robust memory T cell responses akin to those observed in the context of successful vaccines, suggesting that natural exposure or infection may prevent recurrent episodes of severe COVID-19 also in seronegative individuals," the team wrote in the paper.
The study results indicate that public immunity to SARS-CoV-2 infection is potentially higher than antibody tests have shown. However, the team noted that T-cell analyses are more complex and harder to perform. They are conducted in specialized laboratories.
"Larger and more longitudinal studies must now be done on both T cells and antibodies to understand how long-lasting the immunity is and how these different components of COVID-19 immunity are related," Buggert explained.
Global toll
The coronavirus pandemic has now reached another milestone, as more than 10 million have now infected with SARS-CoV-2. The United States reports the highest number of casualties, with a death toll of at least 128,000.
The U.S. has more than 2.68 million confirmed cases, followed by Brazil, with a staggering 1.44 million cases. Russia, India, and the United Kingdom report high infection tolls, with more than 653,000 cases, more than 585,000 cases, and more than 314,000 cases, respectively.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Source:
Journal references:
- Preliminary scientific report.
Sekine, T., Perez-Potti, A., Rivera-Ballesteros, O., Stralin, K. et al. (2020). Robust T cell immunity in convalescent individuals with asymptomatic or mild COVID-19. BioRxiv. https://www.biorxiv.org/content/10.1101/2020.06.29.174888v1
- Peer reviewed and published scientific report.
Sekine, Takuya, André Perez-Potti, Olga Rivera-Ballesteros, Kristoffer Strålin, Jean-Baptiste Gorin, Annika Olsson, Sian Llewellyn-Lacey, et al. 2020. “Robust T Cell Immunity in Convalescent Individuals with Asymptomatic or Mild COVID-19.” Cell 183 (1). https://doi.org/10.1016/j.cell.2020.08.017. https://www.cell.com/cell/fulltext/S0092-8674(20)31008-4.