The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is still spreading across the globe, nearly 11 million cases, and more than 519,000 deaths so far. In the absence of any effective pharmaceutical interventions, such as a vaccine or antiviral, measures such as lockdowns, social distancing, and the mandatory use of face masks and careful hand hygiene govern the response to the pandemic. These are collectively called non-pharmaceutical interventions (NPI).

Study: Quantifying the impact of US state non-pharmaceutical interventions on COVID-19 transmission. Image Credit: PowerUp / Shutterstock

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Quantifying NPI Impact on Transmission
Now, a new study published on the preprint server medRxiv* looks at how the effects of these NPIs can be quantified in order to keep the public health response to COVID-19 at an adequate level. While NPIs are known to reduce the peak of the infections, in general, the researchers wanted to quantify different components separately. There is a considerable difference in the way that different regions and governments have applied various NPIs, which makes it difficult to predict the separate benefit of each by itself.
However, these differences do allow the impact of measures applied in the past to be assessed on the basis of the already observable impact. The researchers used statistical methods along with the mortality data to arrive at insights about the changes in the rate of transmission over time subsequent to the NPI applied.
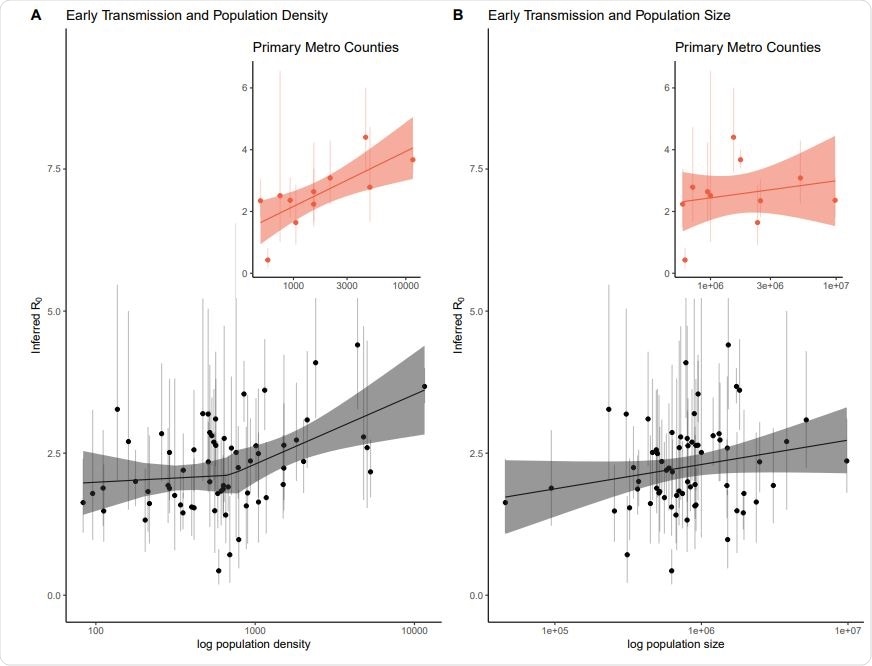
Early epidemic estimates of R0 with 95% quantile bars against population density and population size. Panel A plot R0 against population density with the best fit segmented linear regression line and 95% confidence bands. We fit the linear model allowing for one breakpoint in population density. The best-fit cut point is around population density just under 1,000. The association between density and R0 is not significantly below this cut point but is statistically significant for densities above ∼ 1,000 people per square kilometer. Additionally, to account for commuter effects, we extracted the primary county per major metropolitan area across a number of states and the relationship between population density and R0 is statistically significant for these counties. Panel B plots R0 against population size with a linear fit through the association was not significant. The subset of primary metropolitan counties is plotted as well, with the (not significant) best-fit line. We found a positive relationship between population density and R0. In contrast, we found no relationship between population size and R0, indicating that highly dense areas are at greater risk of rapid spread, while less dense areas may require comparatively fewer interventions to slow the spread of the virus.
Classifying NPIs by Severity
The study is based on the use of response ranking criteria to provide a more convenient structure for the data, with responses being classified as pre-NPI, or no response, and low, medium, and high response depending on how many contacts were reduced with each change in policy.
Low-level responses included emergency states and mild restrictions on public gatherings of 500-1,000 people; medium-level responses include restrictions to 25-100 people, closing down schools, and certain limitations on dining and retail shopping; high-level responses include shelter in place orders in a region or a state, closure of restaurants, bars and shops, and restrictions on public gatherings of 10 people or more.
The researchers estimated the basic reproductive value R0, at the beginning, and the time-dependent transmission rate in over 670 people. They also examined the impact of population density, which differs in each situation, on the early exponential growth of the pandemic. After adjusting for biases and confounding factors, they found that R0 is positively correlated with a higher density once the threshold is crossed, and the stricter the interventions, the more the magnitude of reduction in transmission.
Population Density Increases Transmission Rate
They examined 65 counties with early exponential growth and a sufficient number of deaths to allow a reliable R0 calculation using the mortality data. These were spread over 24 states. The population density was also calculated in terms of the actual density, leaving out thick woods and water bodies. They also adjusted for commuters into a very densely populated county from a less dense neighboring county.
They found a strong relationship between the density of population and R0, with a significantly more rapid transmission in higher density areas. This means that in such areas, quick and firm action must be taken to enforce NPIs to reduce viral spread effectively. This relationship is significant at a threshold of just below 1,000 people per square kilometer.
Stronger NPIs Reduce Transmission
Secondly, they found that with more intensive NPIs, R0 declines, and viral spread is reduced as well.
In other words, they say, “These results suggest that proactive state-wide measures are a highly effective way to limit the spread of COVID-19 and that stronger measures are associated with significantly reduced disease spread.”
Interestingly, the Southern and Western states currently showing a rapid or even record increase in daily case counts are those which did not show a marked reduction in Re even under the most intensive restrictions. This suggests that this surge was perhaps operating even before the current relaxations were granted.
Again, comparing different counties showed that the most significant gain in the reduction of viral spread comes from moving from no NPI to the lowest level of NPI, that is, restricting large gatherings, which are considered superspreader events. However, it does not stop the outbreak. With higher time-varying values of transmission, the reduction is steeper following the application of an NPI.
Implications and Importance
The researchers also point out that these findings indicate the U.S. never actually experienced an arrest of the outbreak, with the R0 less than one. This is probably, they write, “a result of rolling back social distancing guidelines and comparative leniency and inconsistency in both U.S. policy and policy enforcement at the state level.” There has been considerable public agitation and state resistance against social distancing and even the wearing of masks, which has hampered the aggressive implementation of NPIs, unlike the events in South Korea and New Zealand, for instance.
The findings could help evaluate control measures in place, as well as provide a longer-range lens to discover how such strategies can be tuned over time to allow adaptive restrictions as and when transmission crosses a threshold.
The researchers sum up: “These results shed light on the effective role of rapid and robust state-level NPIs, crucial in the absence of widely available therapies or vaccines.”

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.