Numerous studies have described the demographics, coexisting illnesses, and outcomes among patients hospitalized with COVID-19 disease. However, there are many more patients who have symptomatic disease but do not go to hospital. Thus, hospitalized patients are not an accurate reflection of the total numbers of infected individuals, especially since COVID testing is also often focused on those who are at risk or present with symptoms.
The problem with this is that this makes it more challenging to identify the specific risk factors that increase the risk of progression.
The Study: Overview of COVID-19 Statistics
The current study aims to provide a full-spectrum picture of patient data in terms of incidence of symptomatic cases, their follow-up over a time frame, and identification of the outcomes of these patients, including whether they had to be hospitalized, or they died.
The researchers also gathered data on chronic health conditions so they could analyze the impact of such disease on the course of COVID-19, using linked real-world data. The setting of this study in Catalonia, where primary health care is universal and free, and the first contact with the health system is with the general practitioner, even with the onset of COVID-19, makes it possible to retrieve all this data from the health records.
The study included all individuals enrolled in the Information System for Research in Primary Care (SIDIAP). This provides records of primary care for more than 80% of the inhabitants of Catalonia and is linked to the records of regional COVID-19 testing, hospital and death records. The study period was between March 1 and May 6, 2020.
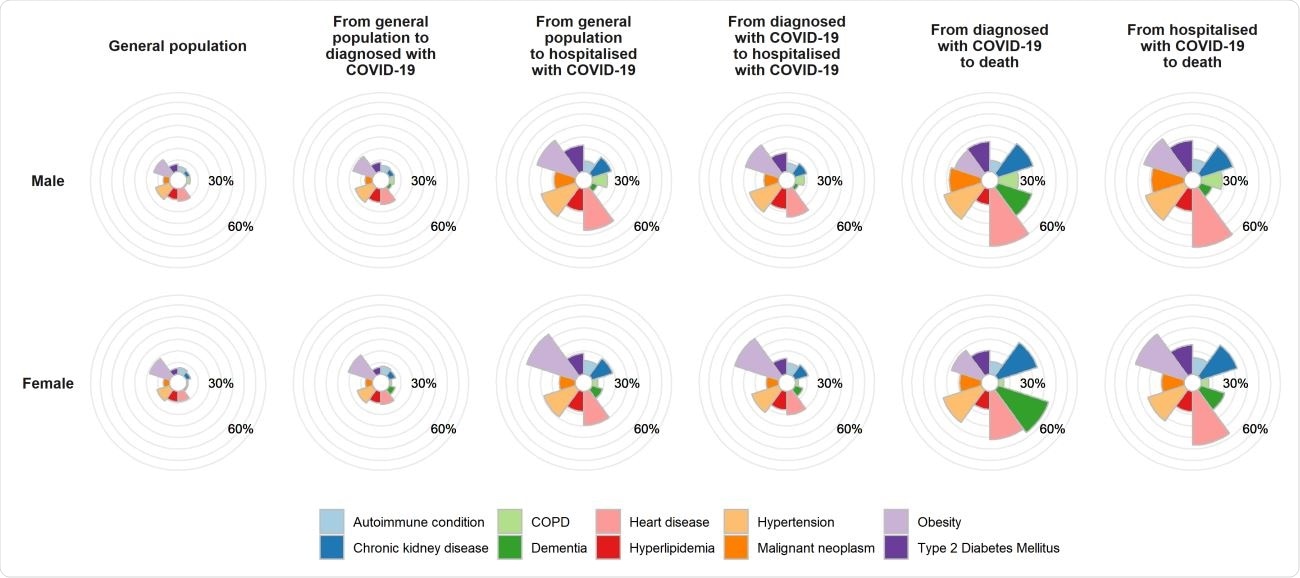
Prevalence of comorbidities in COVID-19 affected and general population

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Incidence and Mortality
Of more than 5,600,000 registered individuals, there were over 109,000 confirmed outpatients with COVID-19, which comes to about 2% of the population. Just over 18,000 people were hospitalized with COVID-19, and 5,585 died after either being diagnosed or hospitalized with COVID-19. Half of those who died were not admitted to hospital prior to their death. Among hospitalized patients, about 19% died within 45 days from follow up.
The median age of the population was 44 years, but of the COVID-positive population 47 years. And for those hospitalized with symptomatic disease after or before first being diagnosed as outpatients, the median age was 61 and 72 years, respectively.
For deaths outside hospital, the median age was 87 years, and 81 years for those who died in hospital.
Risk Factors: Age
The highest number of diagnoses came with middle age, at around 45 years, and then at the oldest ages. As expected, compared to the risk at 65 years, the risk at 20 years was 31% less, 62% greater for a 45-year-old, and 113% greater at 90 years. The highest risk of being hospitalized after a COVID-19 diagnosis was at the age of 70 years.
All other outcome risks were highest with advancing age, including deaths in or out of hospital, and in males. A 90-year-old would have three times the risk of being hospitalized with this diagnosis on initial presentation, compared to a 65-year-old, a six-fold risk of death while in hospital, and 17 times the risk of dying out of hospital after being diagnosed. Conversely, a 20-year-old would be at less than a hundredth of the risk at 65 years.
Risk Factors: Male Sex
More males were diagnosed with symptoms severe enough to be hospitalized straightaway, and among those with an outpatient diagnosis, more males eventually were in hospital. However, more females died outside hospital after diagnosis. Overall, 60% of deaths were in males.
The adjusted risk for males was lower for outpatient diagnosis, at 25% less compared to females. However, they were at 60% higher risk for direct hospitalization with this condition, 82% higher for hospitalization after prior outpatient diagnosis, 75% increased risk of death after an outpatient diagnosis, and 41% higher for death in hospital. However, at 70 years old, females were at a still higher risk of dying with this diagnosis.
Risk Factors: Chronic Disease
Chronic health conditions recorded in the diagnosed individuals were all predictive of poorer outcomes. All these conditions, like chronic kidney disease, chronic obstructive pulmonary disease, obesity, and type 2 diabetes, which exists at prevalences of 4% to 17% depending on the condition, were at 14% to 40% among the fatalities due to COVID-19. The risk of COVID-19 diagnosis was higher by 8% to 16% with these conditions.
Obesity and dementia were linked to a 74% and 82% increase in the likelihood of hospitalization in individuals not previously diagnosed with COVID-19. Obesity increased the risk for later hospitalization among COVID-positive cases by 60%.
About 60% of women who died outside hospital with COVID-19 had dementia, and overall, 40% of all deaths among non-hospitalized COVID-positive patients were in dementia patients. In other terms, the adjusted risk for death outside hospital for dementia patients was 92% higher. The reasons range from the occurrence of severe outbreaks within these nursing homes, greater surveillance of these homes, and the barriers to obtaining or seeking care for these patients.
Implications
The study shows that those who are at the highest risk of poor outcomes continue to be the elderly. At the same time, those who develop symptomatic COVID-19 will require to be hospitalized earlier if they show any signs of progression, to avoid fatal outcomes.
The researchers comment, “This may reflect rationing of health care resources, with younger patients likely prioritized for the receipt of hospital care, and intensive services if admitted. With half of the deaths in this study observed among those not hospitalized after diagnosis, who had an average age of 87, it is of utmost importance that similar individuals should be given appropriate access to care in the future.”
While those who are younger have lower risks of hospitalization and death, they can spread the virus through the community. Therefore, public health policies must be tailored to minimize this role by encouraging vaccination and social distancing.
Source
Burn, E. et al. (2020). The Natural History of Symptomatic COVID-19 In Catalonia, Spain: A Multi-State Model Including 109,367 Outpatient Diagnoses, 18,019 Hospitalisations, And 5,585 COVID-19 Deaths Among 5,627,520 People. medRxiv preprint. doi: https://doi.org/10.1101/2020.07.13.20152454. https://www.medrxiv.org/content/10.1101/2020.07.13.20152454v1

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Burn, E. et al. (2020). The Natural History of Symptomatic COVID-19 In Catalonia, Spain: A Multi-State Model Including 109,367 Outpatient Diagnoses, 18,019 Hospitalisations, And 5,585 COVID-19 Deaths Among 5,627,520 People. medRxiv preprint. doi: https://doi.org/10.1101/2020.07.13.20152454. https://www.medrxiv.org/content/10.1101/2020.07.13.20152454v1
- Peer reviewed and published scientific report.
Burn, Edward, Cristian Tebé, Sergio Fernandez-Bertolin, Maria Aragon, Martina Recalde, Elena Roel, Albert Prats-Uribe, Daniel Prieto-Alhambra, and Talita Duarte-Salles. 2021. “The Natural History of Symptomatic COVID-19 during the First Wave in Catalonia.” Nature Communications 12 (1): 777. https://doi.org/10.1038/s41467-021-21100-y. https://www.nature.com/articles/s41467-021-21100-y.