The current severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), causing the pandemic of COVID-19, has not met its match by way of an effective vaccine or antiviral. However, several risk factors have been identified, one of which is obesity. Statins are a class of drugs often used to control high cholesterol levels in obesity. Now, a study published on the preprint server medRxiv* in July 2020 suggests that statins do not aggravate the risk of COVID-19 infection and may have a small beneficial effect in some cases.
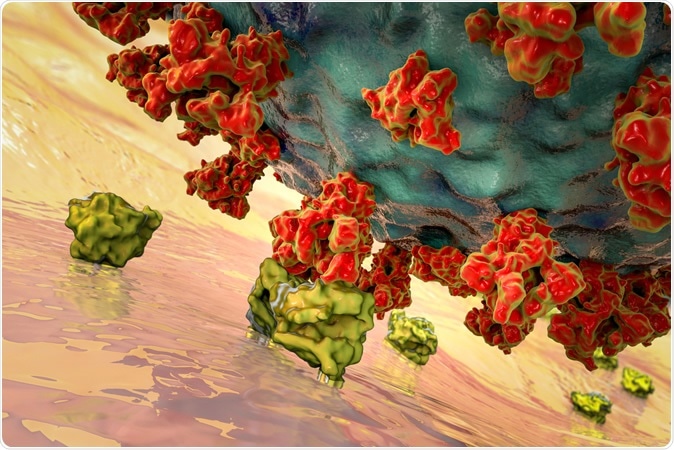
SARS-CoV-2 viruses binding to ACE-2 receptors on a human cell, the initial stage of COVID-19 infection, conceptual 3D illustration credit: Kateryna Kon / Shutterstock
Statins are most commonly prescribed to reduce cholesterol levels and inflammation in individuals with hypercholesterolemia, type 2 diabetes, and cardiovascular disease, including ischemic heart disease and stroke. They make up an astounding number of prescriptions at 26% of all Americans over the age of 40 years and up to 40% of all German type 2 diabetes patients. Thus, a considerable proportion of older adults take them.
This same population group is at particular risk of contracting SARS-CoV-2, and of developing severe disease following virus exposure. Prior retrospective analysis has suggested that COVID-19 patients who are on statins fare better clinically than others.
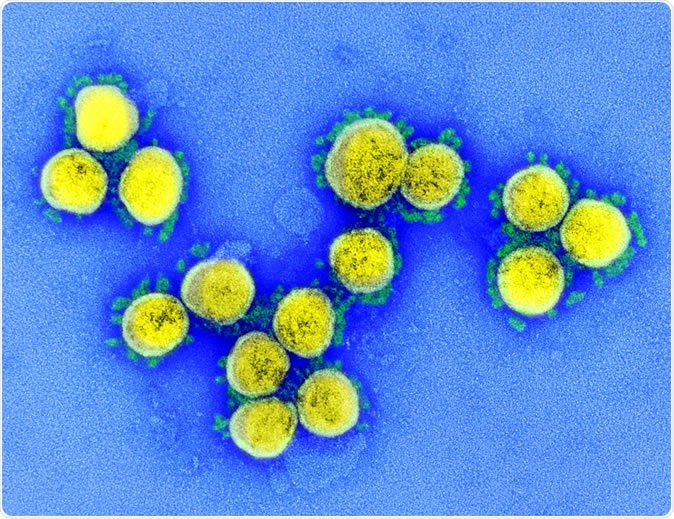
SARS-CoV-2 - Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
Statins work by inhibiting the activity of the HMG-CoA enzyme, a crucial component of the cholesterol biosynthesis pathway. SARS-CoV is known to depend heavily on its intact membrane, with cholesterol-heavy microdomains, to bind efficiently to the host cell receptor, the angiotensin-converting enzyme 2 (ACE2).
SARS-CoV-2 also uses the same receptor, which led to curiosity as to the possible impact of these drugs on the entry of the virus into the cell. The current study aimed to examine the effect of statins on the outcome of COVID-19 as well as to determine their impact on the entry and replication of the virus. The researchers here used cell cultures and pseudotyped vesicular stomatitis virus (VSV), expressing the spike protein of the SARS-CoV-2, to examine how the virus infectivity differed after statin exposure.
Reduction of Alphacoronavirus Entry
They found that the alphacoronavirus 229E (of low pathogenicity) showed a moderate reduction in infectivity at 5 μM of statin concentration. The most significant effect was with Fluvastatin. This drug was able to reduce the infection in a dose-dependent manner, and the IC50 was 9.8 μM. At all the tested doses, Fluvastatin did not produce any evidence of cell toxicity, with 80% or more of cells remaining viable.
When pretreated with Fluvastatin at 10 μM, the entry of the virus was reduced fivefold, but not of viral particles that cannot bind to ACE2. The more frequently used drugs, simvastatin, atorvastatin, lovastatin, pravastatin, and rosuvastatin also caused slight but insignificant reductions in the 229E assay.
Reduction of Betacoronavirus Entry
Chloroquine, however, blocked infection effectively with SARS-CoV-2 but not with SARS-CoV, because the latter undergo cleavage of the spike protein at the plasma membrane rather than in the endosomes. When cyclodextrin was added to reduce cholesterol levels, both SARS-CoV and SARS-CoV-2 entry was reduced but not the VSV pseudoparticle. This offers a possible explanation for the mechanism of action of statins on viral entry into the respiratory epithelial cells.
When Fluvastatin at 10 μM dosage was used to pretreat human respiratory epithelial cells before exposing them to a highly pathogenic strain of SARS-CoV-2, the scientists observed a moderate reduction in viral genome copies. Thus, there is no enhancement of COVID-19 infection risk in patients on statins, as suspected earlier. Instead, some statins may be able to reduce viral entry and infection in vitro.
Retrospective Study: Low HDL in Older Patients, Increased Mortality
The researchers also carried out a retrospective analysis of 65 severely ill COVID-19 patients in the intensive care unit (ICU), with 3 each on simvastatin and atorvastatin. Eight of them had low high-density lipoprotein (HDL) cholesterol levels below 20 mg/dL.
The median age of the patients overall was 63 years, but of the eight with low HDL, 73 years. Most were male. The median ICU stay duration was 12 and 16 days, respectively. Seven of the eight low-HDL patients died, but 14/57 remaining patients. Those of an age-matched cohort matched the results in the low-HDL group.
Low HDL has been reported in critical COVID-19 patients. Since statins increase HDL levels while reducing LDL levels, their lipid homeostatic effect may contribute to their beneficial effect in this pandemic viral infection.
The Implications
The researchers speculate: “As statins reduce LDL and may increase HDL levels, statin modulation of serum lipoprotein homeostasis may –in addition to immunomodulatory and other yet unknown effects - contribute to the previous observations of beneficial effects of statins in patients.”
They note that in keeping with the beneficial effect of statins on the progression of COVID-19 to severe disease, the study showed moderate inhibition of both alpha- and beta-coronaviruses in vitro. However, the concentrations of Fluvastatin used were at least one magnitude higher than serum levels in the typical patient and much more than that likely to be found in the respiratory tract.
In other words, the direct inhibitory effect may not be observed in patients. Moreover, the pseudoviruses used in the current study did not express the SARS-CoV-2 protease, which is essential for viral entry.
Instead, statins may make the immune response more effective and thus reduce the severity of the infection. Statins have been observed to have an immunomodulatory effect on neutrophils in patients with pneumonia and other infections. Further research is needed in animal models to find out how this occurs.
Another mechanism suggested is that the reduction of membrane cholesterol prevents normal ACE2-spike interactions.
Overall, they say, “Cumulative data from this and other studies strongly argue that individuals on statin therapy can continue statin regimen during the current SARS-CoV-2 pandemic.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources