Physicians working at Cambridge University Hospital NHS Foundation Trust have reported that a significant proportion of patients with severe coronavirus disease 2019 (COVID-19) who required intensive care developed unanticipated disabling neurological deficits that were related to a mononeuritis multiplex.
Mononeuritis multiplex or multifocal neuropathy is a form of peripheral neuropathy that involves inflammation of two or more different nerve areas. It can cause asymmetrical sensory and motor damage in multiple parts of the body.
Stephen Sawcer and colleagues say it is expected that many survivors of severe disease who need to be supported with long-term mechanical ventilation may be left with significant Intensive Care Unit – Acquired Weakness (ICUAW).
“However, in our post-COVID-19 follow up clinic, we have found that, as well as the anticipated global weakness related to loss of muscle mass, a significant proportion of these patients also have disabling focal neurological deficits relating to an axonal mononeuritis multiplex,” they write.
The team says this unexpected complication of severe COVID-19 could have significant long-term impacts on outcomes for many patients and profound implications in terms of their rehabilitation needs.
Sawcer and colleagues strongly recommend that COVID-19 survivors who have ICUAW undergo detailed neurological assessment since many are likely also to have the focal neurological deficits.
A pre-print version of the paper is available on the server medRxiv*, while the article undergoes peer review.
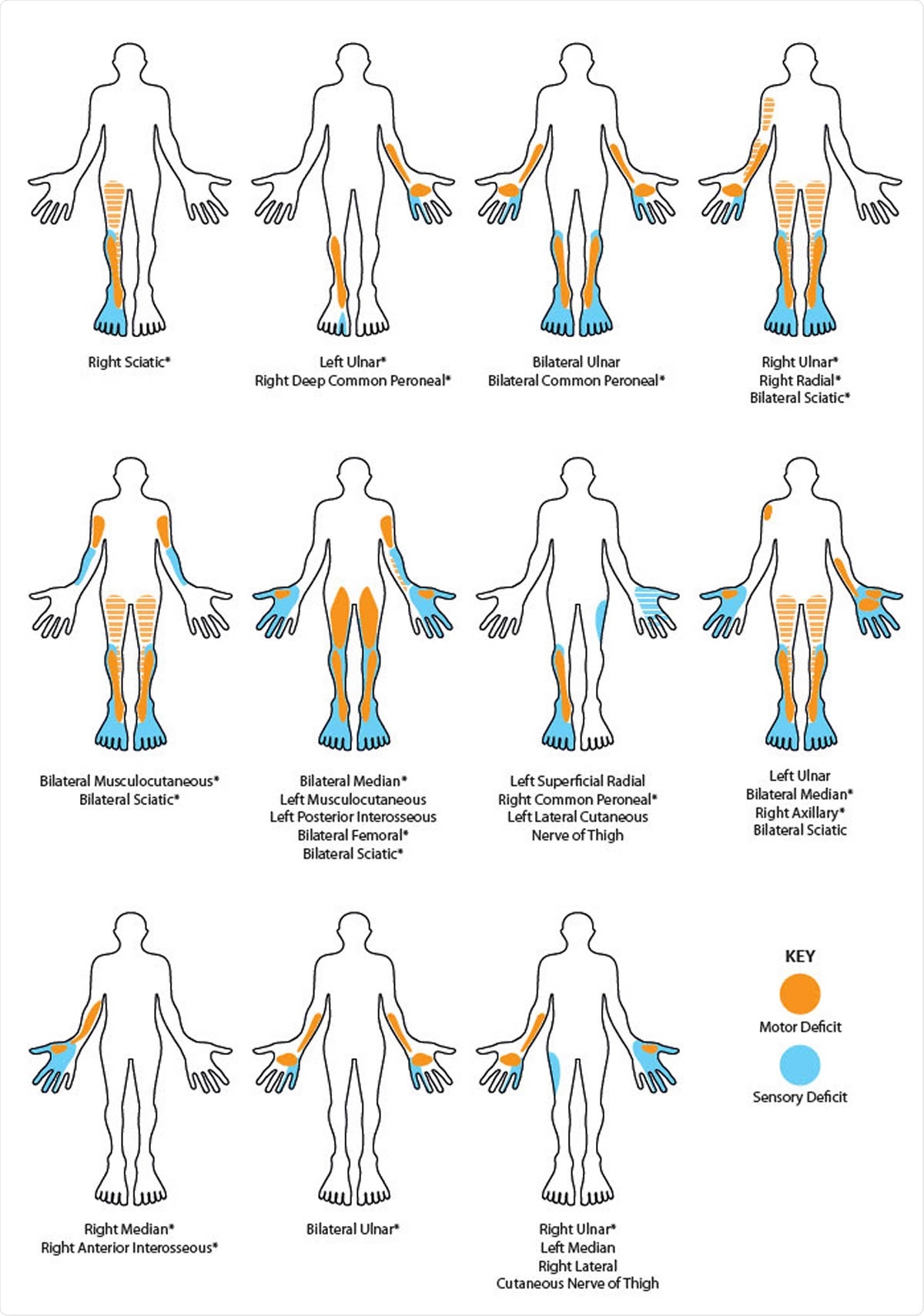
Schematic homuncular illustration of the sensory and motor deficits arising from the multiple mononeuropathies present in eleven patients recovering from severe COVID-19. * denote those neuropathies which were unequivocally confirmed electrophysiologically. Hatched shading indicates posterior muscle groups (hamstrings and triceps). In those neuropathies listed as sciatic there was involvement of both common peroneal and tibial divisions.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Complications associated with prolonged respiratory support
The respiratory complications associated with COVID-19 have placed a significant strain on healthcare services globally. Many patients need prolonged respiratory support with mechanical ventilation, which can result in significant ICUAW.
Now, Sawcer and team have found that among patients attending the hospital’s post-COVID-19 follow-up clinic, a significant number not only experience the global symmetric weakness related to loss of muscle mass and strength, but also significant neurological deficits related to multifocal neuropathy.
Eleven (16%) of 69 survivors who had been discharged from intensive care after receiving prolonged mechanical ventilation (average period 31 days) had this type of neuropathy. The team says that in many cases, the global symmetrical weakness observed had initially been assumed to be related to critical illness neuropathy. However, a detailed neurophysiological assessment identified axonal sensorimotor mononeuropathies, and critical illness neuropathy was only seen in one patient.
The nerve involvement was often random, with some nerve fascicles (which are made up of bundles of axons) more significantly affected than others. Three patients underwent ultrasound scanning, which showed widespread thickening of the nerves that had been affected.
One patient with bilateral femoral neuropathies underwent an MRI scan. That scan revealed the presence of bilateral psoas hematoma, which is a complication of extracorporeal membrane oxygenation (ECMO). ECMO is a type of respiratory support that involves blood being pumped to a heart-lung machine where carbon dioxide is removed and oxygen added before blood is returned back to the body.
However, “this finding did not explain the upper limb nor the sciatic neuropathies,” reports the team.
A patient with bilateral sciatic nerve lesions also underwent an MRI scan, but the nerves appeared normal, and an MRI scan of the brachial plexus in another patient showed that the nerves were normal.
Additional cases of mononeuropathy may still emerge
Sawcer and colleagues say that to date, 102 patients with COVID-19 have been treated in the hospital’s intensive care units. Forty-four have been discharged; 14 have been moved to other hospitals; 11 are still recovering, and 33 have died. Since not all patients have been discharged, additional cases of mononeuropathy may still emerge in the weeks to come, the team adds.
“This series highlights an important neurological complication of COVID-19, which detrimentally affects the long-term outcomes of patients and markedly influences their rehabilitation needs,” writes Sawcer and colleagues. “Given that this complication is evident in a significant proportion of the patients discharged from the intensive care units of a single hospital (16% in our cohort of treated patients), the rehabilitation burden globally could be substantial.”
The team also points out that, since cases of ICUAW will be expected, the focal deficits observed here may also go unrecognized.
Sawcer and colleagues say they acknowledge that overall, the number of affected patients is small and that their observations have not involved a comparative group. However, the clinical features are “striking” and have important implications for patients’ outcomes and their rehabilitation.
“We strongly urge detailed neurological assessment of patients with post-COVID-19 ICUAW, especially those with asymmetric weakness, as we suspect that many such patients are likely to have focal deficits resulting from their COVID-19 illness,” they conclude.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Sawcer S, et al. Mononeuritis multiplex: an unexpectedly common feature of severe COVID-19. medRxiv 2020. doi: https://doi.org/10.1101/2020.07.19.20149898
- Peer reviewed and published scientific report.
Needham, Edward, Virginia Newcombe, Andrew Michell, Rachel Thornton, Andrew Grainger, Fahim Anwar, Elizabeth Warburton, David Menon, Monica Trivedi, and Stephen Sawcer. 2020. “Mononeuritis Multiplex: An Unexpectedly Frequent Feature of Severe COVID-19.” Journal of Neurology 268 (8): 2685–89. https://doi.org/10.1007/s00415-020-10321-8. https://link.springer.com/article/10.1007/s00415-020-10321-8.