The world went into lockdown mode when it was faced with the threat of a rapidly spreading and sometimes fatal respiratory viral infection, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The virus first cropped up in China’s Wuhan city in Hubei province, and then crossed the oceans and continents, and was declared a pandemic by the World Health Organization (WHO) on March 11, 2020.
Over the next five months, it caused almost 20 million cases and over 731,000 deaths worldwide. The USA has witnessed a rapid spread of the virus, with the one-hundredth death recorded on March 16, 2020, while currently, it has experienced over 162,000 deaths.
In the absence of any effective vaccine or antiviral preventive or therapeutic drug, the only possible response to an extraordinarily contagious and unknown disease was in the form of multiple non-pharmaceutical interventions (NPIs). China implemented what some describe as a ‘Draconian’ lockdown, with total closure of public transport, and all residents ordered to stay at home.
Similar measures restricting travel, quarantining people with suspected or confirmed disease, and tracing contacts, were put in place in other Asia countries, and a month later, in Europe. The latter was also characterized by school and non-essential closures, limits on the number of people who could gather, bans on international travel, and shelter-in-place mandates. The response in the US was quite different in many ways. For one thing, both state and local authorities decided on the measures to be taken.
Overall, in most affected areas, stay-at-home orders were passed by March 21, 2020. In the early part of the pandemic, there was a significant reduction in the number of people moving around places like retail, grocery, workplace locations, pharmacies, and parks. Research focused on this time showed that combinations of NPIs had significant success in lowering viral transmission. The greatest impact was observed with an intensive reduction in contacts, such as lockdowns.
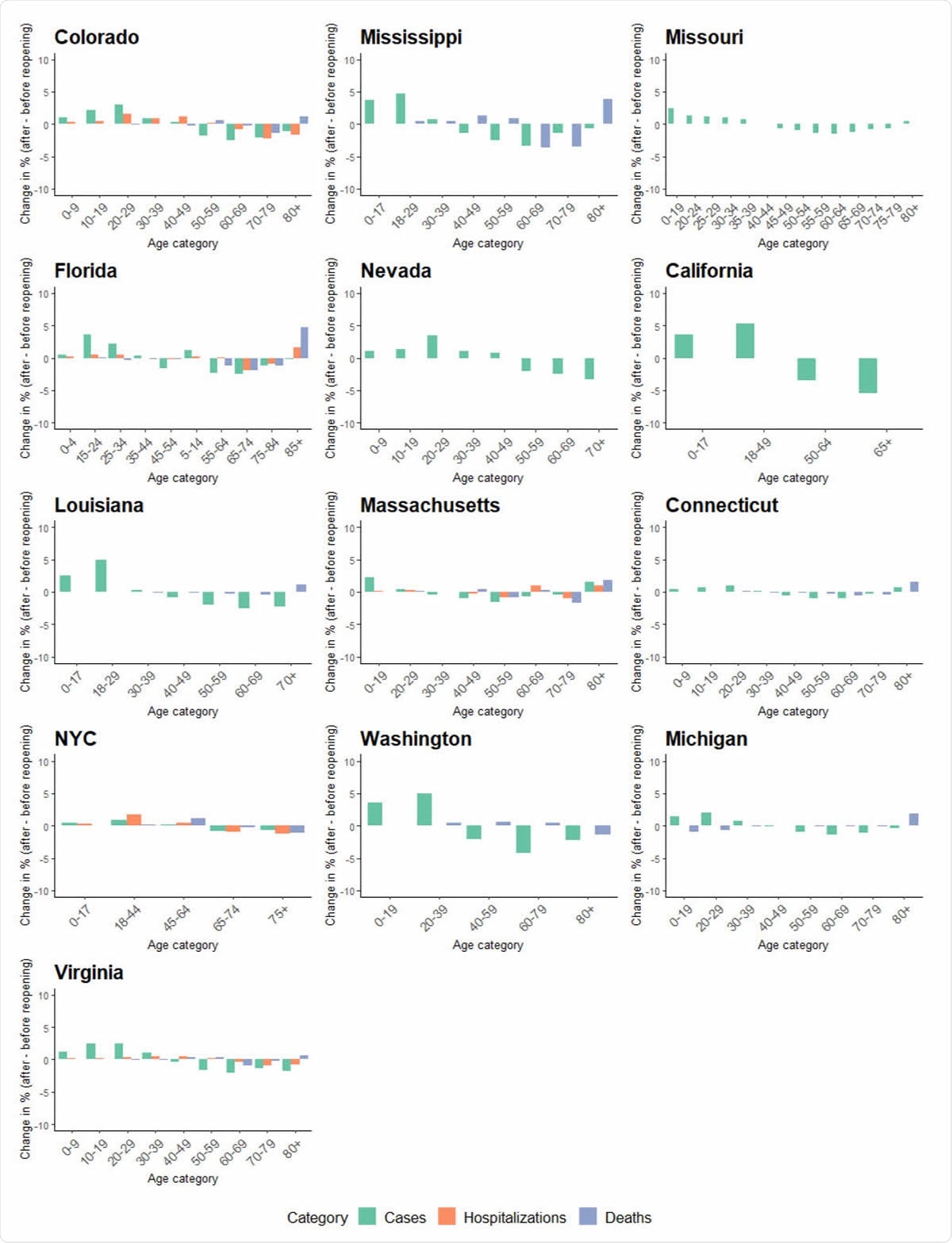
Average share change of age groups on cases, hospitalizations, and deaths before and after reopening in 13 states or regions. States are ordered by reopening date. Death data were available for 10 states and hospitalization data were available for five states.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Pressure to Reopen
Almost from the beginning, the pressure was on to reopen, in view of the high economic impact. The problem was that nobody knew how and when to reopen without provoking a big flare-up and even more deaths. The most consensual view was that reopening should take place in a staged manner, sensitive to the local scenario, rather than an all-or-none strategy.
A major controversy has been over school reopenings since evidence shows that targeted NPIs in different age groups have the best results. However, the supposed educational loss and stress on children and their caregivers have led many scientists to push schools to reopen once the risk of children getting sick or spreading the virus is deemed low.
Again, the outcome of COVID-19 was seen to be markedly affected by age and coexisting disease conditions. In the USA, patients over 65 years made up about 80% of the deaths, from less than 17% of the population. On the other hand, people who were already sick or had chronic diseases had a 6-12 times higher death rate than previously healthy patients.
With gradual relaxations beginning towards the second half of April 2020, culminating in some US states reopening, there was a steep rise in the number of cases in the country. In May 2020, cases rose in some parts of Europe and Asia too.
The current study sought to explore whether the cases that followed reopening had worse outcomes and affected different age groups. The researchers used publicly available time-series data for cases, hospitalizations, and deaths by age in 50 US states and 11 European countries. This is a pioneering study in this area.
Discrepancy Between Rise in Cases and Deaths
The study shows that 8 of 11 European countries had significantly more cases after reopening, but Germany, the UAE, and Poland had fewer. In five of the eight, the cases increased, peaked, and then dropped before the reopening happened, while Romania and Serbia showed a rapid rise before reopening. The UAE, surprisingly, had fewer cases after reopening, though the number of cases had gone up before that.
The daily death rates increased in only 2 of these countries, namely, Romania and Serbia, and two had no change (Slovenia and the UAE). The others showed a reduction in daily deaths.
In the USA, 30/40 states had a rise in daily cases, and 10 showed a decrease. The daily deaths increased in seven states only, 14 had no change, while in 19 death went down. The changes in hospitalizations were split almost equally between those which showed increases and decreases.
There were 4 and 15 states and European countries, respectively, which showed the same trend for both cases and deaths per day, after reopening, but 26 states out of 36 had matching cases and hospitalization trends. Also, in contrast to the almost universal trend between cases and deaths before reopening, only two countries and 8 states showed decreases in both parameters after reopening.
The discrepancy between increased daily cases and daily deaths may be real, or apparent due to a lag in recording deaths after case detection, especially when states opened only in June 2020. Another reason could be the recent surge in testing, with more mild cases being picked up now. A third reason could be that as younger patients become sick, the overall mortality falls. And lastly, treatment protocols may be more effective now, improving the overall survival.
Earlier Reopening, Increased Cases
The analysis suggests that earlier reopening is more likely to be associated with increasing new cases. Thus, only about 12% of states who reopened early had a significant drop in infection, but 35% of states who reopened later, after May 15, 2020. Daily deaths, on average, dropped in 61% of late reopening states vs. 29% of early reopening states, matched by a similar trend in hospitalizations.
The major problem in the US was that many states chose to reopen without meeting the predefined criteria, namely, a downturn in flu symptoms, COVID-19 cases, and adequate hospital beds. This has led to a record rise in cases in several states, and some states like California or Florida have now closed again.
What about Age-Stratified Incidence?
After reopening, the elderly (over 60) still made up the majority of deaths due to COVID-19, while those aged 45-60 years accounted for most hospitalizations. The proportion of younger patients, below 40, increased after reopening, but not the proportion of daily deaths.
The changes between European, Asian and US states may not have much significance, since the duration of reopening is quite different in each case. This may be affected by other national characteristics as well. However, letting down one’s guard post-reopening may be a significant factor in increasing the share of younger patients, in all cases. This may not pose a risk to their health, per se, but does exponentially increase the risk to the elderly.
Future Directions
The researchers suggest, “Fast and prepared regional response, including sufficient testing, contact tracing, and tracking, might be the best chance to control the potential spread.”
Spain, in fact, has made the “new normal” decree, mandating the use of face masks, personal protection, and 1.5 m social distancing whenever in a public place.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.