Most individuals infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) develop binding antibodies against viral proteins over a few weeks. The serum dilution required to inhibit viral infection by half is called NT50 and is in the range of 100 to 200 within about a month of symptom onset. However, in some cases, the titers are undetectable, while in others, they may be over 10,000.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Antibody Formation and Decline
The current research is focused on the levels of antibodies in patients who have recovered from COVID-19 disease. Prior research shows that antibodies against the spike protein of the virus fall several-fold from a peak to a few weeks after the onset of symptoms. At this time, the antibody response follows the same trend as with other acute viral infections.
The researchers in this study show that the neutralizing antibodies fall fourfold from 30 to 90 days from symptom onset. At the same time, there is a decrease in titer of spike-binding antibodies and those which bind the receptor-binding domain (RBD). However, the level of neutralizing antibodies remains substantial at 3-4 months from infection.
The study included 34 individuals, of which five were symptomatic and hospitalized, 22 had milder symptoms, while seven were asymptomatic. This cohort had more females than males. The researchers used spike-pseudotyped particles, measuring neutralizing antibody titers over time.
Neutralizing Antibody Titer
In most cases, detectable neutralizing antibodies were found at one month from the first symptom, with NT50 over 20. They found a significant decline in the titer over 30 to 60 days, and past 90 days, the median neutralizing titer was four times less than at 30 days but still at detectable levels. Those patients who had required hospitalization had higher antibody levels early in their convalescence, at both 30 and 60 days.
After this period, from 30 to past 90 days, there was an 18-fold decrease in the neutralizing titer for symptomatic patients who were in hospital, but a threefold fall in the NT50 for those who were not hospitalized. Thus, after 90 days from symptom onset, the neutralization titer was no longer different between patients who had more or less severe disease. Asymptomatic individuals had neutralization titers, which were similar to those of mildly symptomatic individuals throughout the recovery period.
In short, the exaggerated antibody response in severe disease wanes over time, with the resulting fall to more normal levels being correspondingly more obvious than with those patients who had less severe illness.
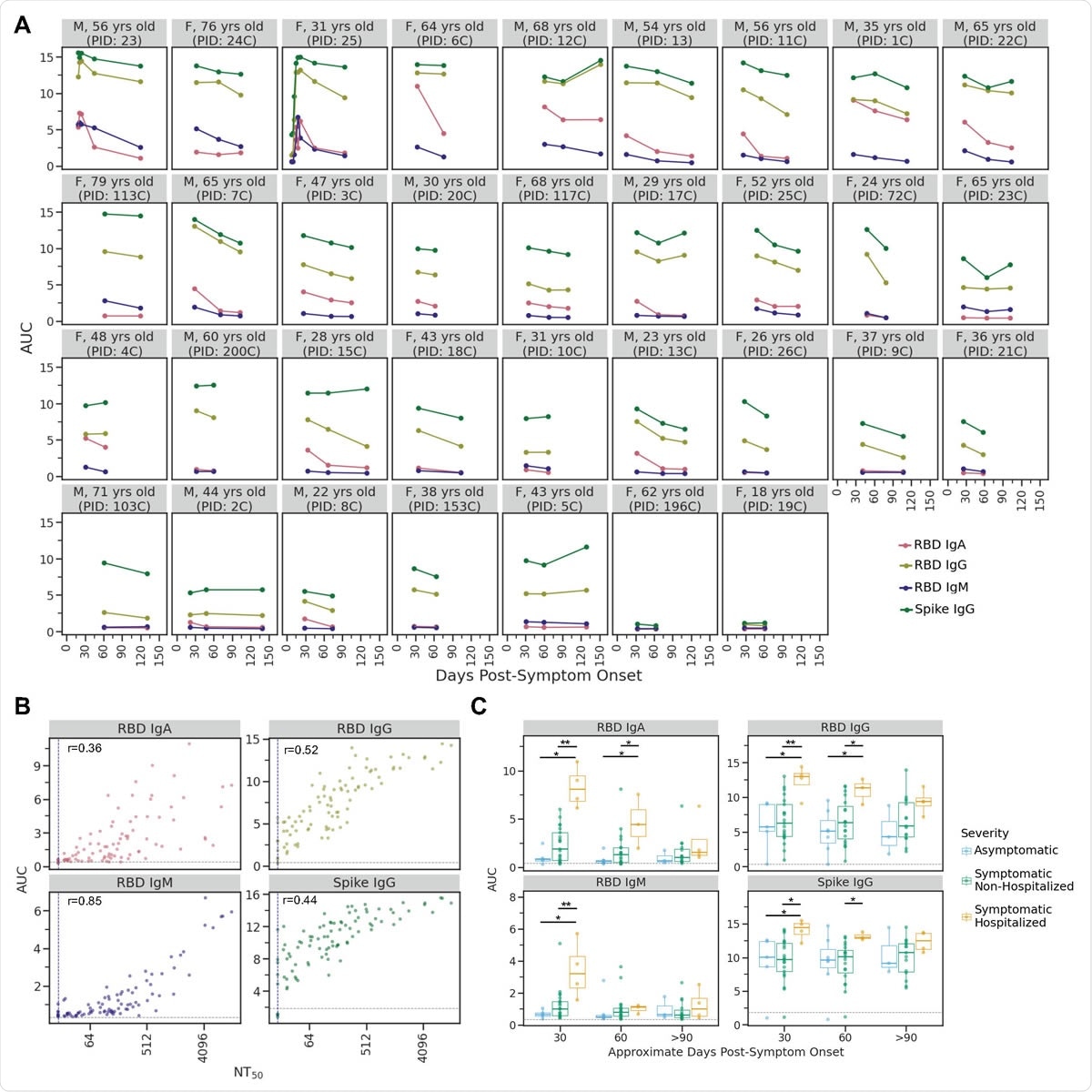
IgA, IgM, and IgG antibody binding titers over time. A) Longitudinal binding antibody titers for each individual as quantified by area under the curve (AUC) of ELISA assays. Facets are arranged by maximal NT50 from top left to bottom right as in Fig. 1A. B) Correlation plots between AUC for each ELISA assay and neutralization titer (NT50) for all samples. The grey line in each facet indicates the AUC value for the negative control sample (2017-2018 sera pool) for each assay. C) For each antibody type measured, individuals who were symptomatic and required hospitalization as part of their care had significantly higher antibody levels during the first one to two months post-symptom onset. *p≤0.05, **p≤0.01. P-values were calculated using the Wilcoxon rank-sum test. As in B, the grey line in each facet indicates the AUC value for the negative control sample for each assay.
Spike- and RBD-binding Antibody Dynamics
With all patients who had to be hospitalized, the IgG, IgA, and IgM binding antibody responses were higher compared to asymptomatic and mildly symptomatic individuals at about 30 days from the earliest symptom. However, at 60 days, the anti-RBD IgM levels were similar in both hospitalized and non-hospitalized patients for any antibody subtype. This trend correlates with that of neutralizing antibodies. Among all patients, IgA and IgM levels went down more steeply than IgG levels between 30 and 90 days from symptom onset.
Implications
The researchers, therefore, conclude that there is no reason for alarm in the decline of antiviral antibody titers over the first few months from symptom onset. They sum up: “While titers decline modestly from ~30 to >90 days post-symptom onset, we found that the dynamics of the antibody response to SARS-CoV-2 in the first several months following infection are consistent with what would be expected from the knowledge of other acute viral infections.”
Further research will be needed to understand how long this immunity will last, which will help to determine how durable is the protection against re-infection with the virus.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources