The COVID-19 pandemic is the defining global health crisis of our time and the most significant challenge we have faced since World War Two. Coronavirus disease 2019 (COVID‑19), is caused by severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2), a highly virulent novel coronavirus, which has caused over 751,000 deaths globally since its emergence at the end of 2019 in Wuhan, the most populous city in Central China.
Health systems are facing unprecedented circumstances and pressure during the COVID-19 as they race to contain the spread of the virus. As the pandemic spreads worldwide, intensive care unit (ICU) practitioners, hospital administrators, governments, policymakers, and researchers must prepare for a surge in critically ill patients. The universal use of personal protective equipment (PPE) at some level, along with the need for physical distancing, has led to excessive strain on hospitals and healthcare workers, and an enormous social and economic toll.
Scientists have been trying to discover new or repurposed drugs to fight this infection and improve the outcome in severe cases. However, most attempts have been unsuccessful. Now, a new study by researchers at Yale University and published on the preprint server medRxiv* in August 2020 reports that the use of two drug categories, namely, JAK inhibitors and Type I interferons (IFNs), is associated with a dramatic improvement in mortality in COVID-19.
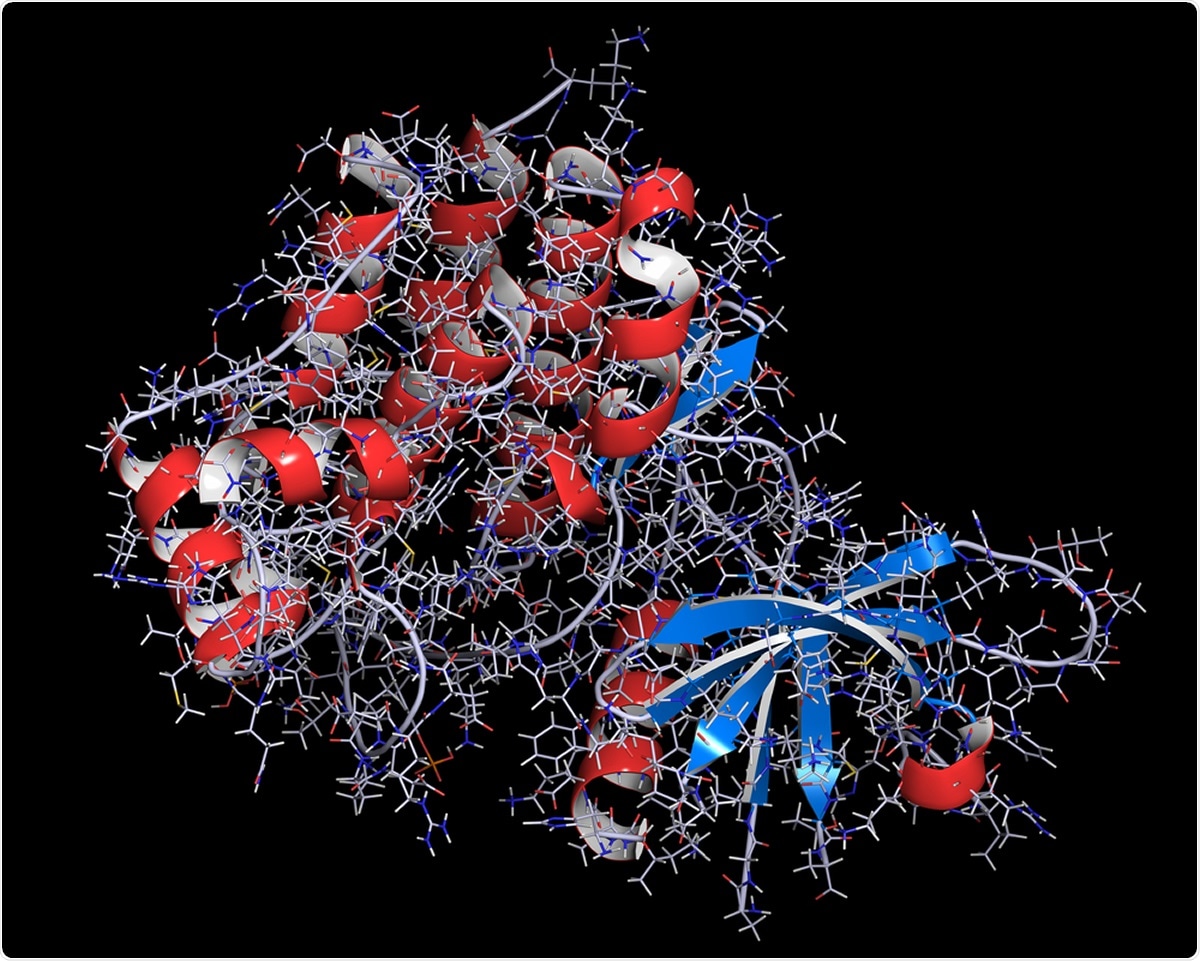
Janus kinase 1 protein. Part of JAK-STAT signalling pathway and drug target. Image Credit: StudioMolekuul / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
JAK Inhibitors
Janus-kinases (JAKs) are transmembrane proteins that are required for and increase the intensity of signals from growth factors and cytokines to host cells. Inhibitors of these proteins thus help to reduce the level of inflammation by bringing down the cytokine levels. Each of these drugs targets a specific JAK, such as baricitinib and ruxolitinib, which inhibit JAK1 and JAK2, respectively.
Their use in severe COVID-19 is obvious, therefore. They have already been used off-label in conditions mediated by excessive cytokine release. The current study seeks to establish the utility of these drugs in severe COVID-19, therefore, in a larger population.
The study looked at the effect of JAK inhibition used in five studies, including just over 170 patients, on outcomes like mortality, ICU admission, the need for mechanical ventilation, the need for acute respiratory distress syndrome (ARDS), and discharge within 14 days. The researchers found that these drugs produced a dramatic reduction in the odds of dying of COVID-19 by 88%, compared to standard treatment.
Again, the odds of requiring ICU admission fell by 95% in a group of 125 patients on JAK-inhibitor treatment.
Type I interferons
Type I IFN-α/β are protein signaling molecules secreted by infected cells. They promote a state of antiviral resistance in other cells in the proximity and also enhance the production of cytokines. The most potent antivirals are type I and type III IFNs, with their effects being mediated via the JAK/STAT pathway. This leads to the activation of many genes called the interferon-stimulated genes (ISGs) that prevent viral replication at several checkpoints.
Since receptors for type I IFNs are distributed extensively, they have a broad range of antiviral activity by inhibiting viral replication both directly and indirectly through multiple mechanisms. These are useful in treating viral hepatitis as well as SARS and MERS, previous outbreaks of coronavirus disease.
Small studies have shown benefit from the use of type I IFNs along with antivirals, but the current study aims to review the effects in a larger population, which will also show the impact of these drugs on the outcome of COVID-19. And in another analysis of the same number of patients, the odds of being discharged at 14 days were almost 23 times higher.
The meta-analysis conducted over three sets of studies, including 990, 454, and 1480 patients on type I interferon therapy, showed that type I IFN therapy did improve the odds of discharge by 90% while reducing the odds of mortality by 80%. However, this therapy did not reduce the need for ICU admission or mechanical ventilation. The odds of severe or critical disease were also similar to those in patients on standard care.
Implications
Type I interferon therapy as well JAK inhibitors offer a twin approach, limiting early viral replication to reduce the severity of the disease, while reducing the extent of inflammation to a level that reduces harm to the host. This is the first systematic review that looks at the outcome of treatment with these drugs in patients with COVID-19. The strong association observed between these drugs and the drastic fall in mortality and ICU admission odds would indicate the need for further investigation into the potential benefit of these therapies in improving the clinical outcome in patients with COVID-19.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources