The most common symptoms noted for the coronavirus disease (COVID-19), which is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), include fever, cough, and difficulty of breathing. As the pandemic evolves, additional symptoms were reported by those who contracted the infection, such as headache, body pains, nausea, diarrhea, and the loss of smell and taste, among others.
.jpg)
This scanning electron microscope image shows SARS-CoV-2 (orange)—also known as 2019-nCoV, the virus that causes COVID-19—isolated from a patient in the U.S., emerging from the surface of cells (green) cultured in the lab. Image captured and colorized at NIAID's Rocky Mountain Laboratories (RML) in Hamilton, Montana. Credit: NIAID
Now, a team of researchers at the University of Southern California (USC) has revealed the order of symptoms often experienced by those who infected with SARS-CoV-2. Knowing the order of the symptoms may help the patients seek medical help immediately. The research is published in the journal Frontiers in Public Health.
"This order is especially important to know when we have overlapping cycles of illnesses like the flu that coincide with infections of COVID-19. Doctors can determine what steps to take to care for the patient, and they may prevent the patient's condition from worsening," Peter Kuhn, a USC professor of medicine, biomedical engineering, and aerospace and mechanical engineering, said.
The team said after several months since the first case of COVID-19 was reported in China, there are now better treatment options, and identifying patients earlier could reduce hospitalization time.
Spot the symptoms quickly
The coronavirus pandemic has negatively impacted the world. It is still unclear when the pandemic will stop, but without treatment and a vaccine available, adapting to a new normal is essential.
Currently, the best way to combat the spreading virus is to spot the symptoms quickly and undergo testing. From there, contact tracing will make sure everyone has been isolated. If patients with symptoms quickly underwent testing and contact tracing, outbreaks could be contained. The drawback is, COVID-19 patients have similar symptoms to common diseases, such as flu and common colds.
"Here, we hypothesize the order of symptom occurrence could help patients and medical professionals more quickly distinguish COVID-19 from other respiratory diseases, yet such essential information is largely unavailable," the researchers explained.
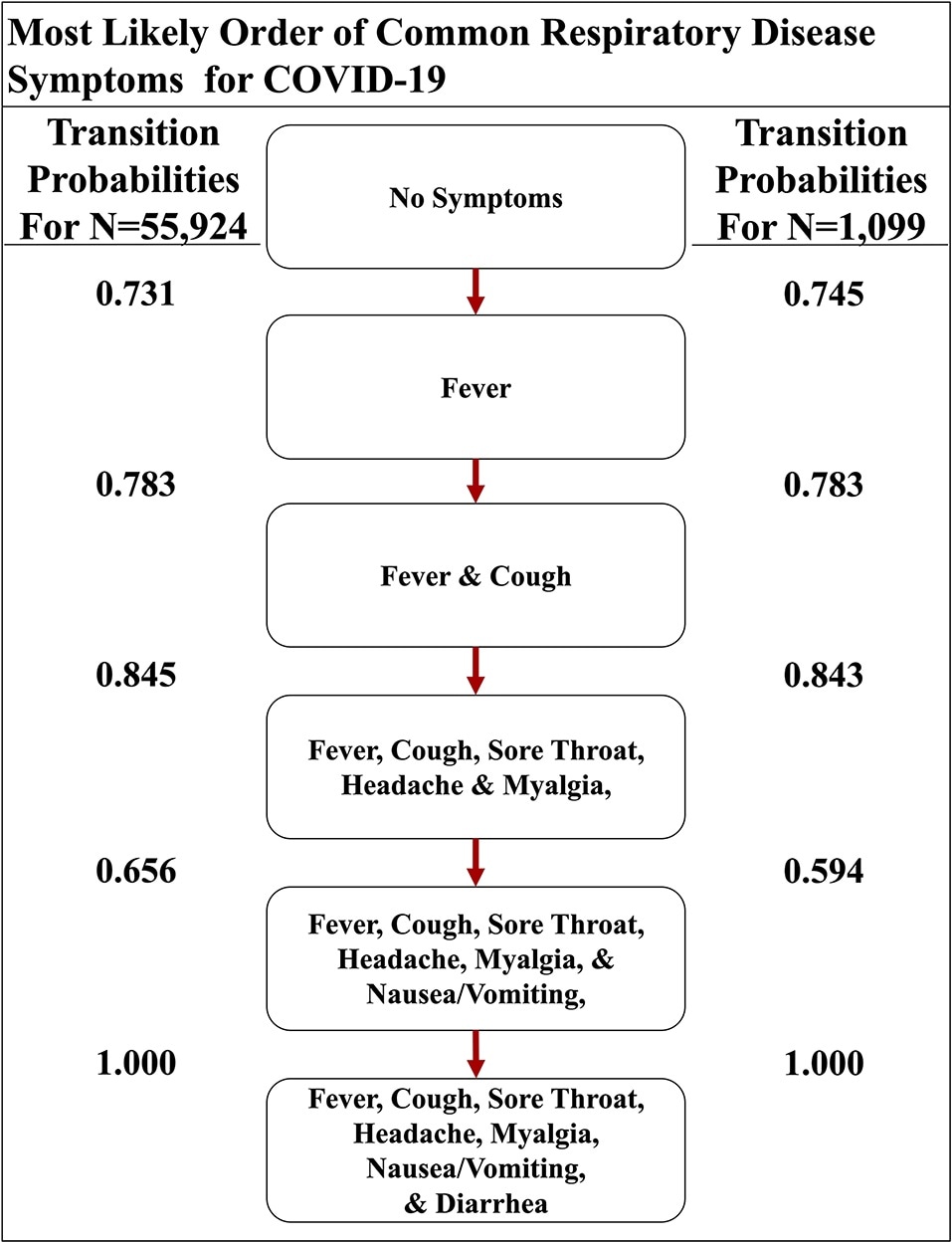
The most likely path of common respiratory symptoms in COVID-19. The most likely path of seven common symptoms of COVID-19, determined by the transition probabilities that are also listed between nodes, of two datasets here. image Credit: Front. Public Health, 13 August 2020 | https://doi.org/10.3389/fpubh.2020.00473
The study
To arrive at the findings of the study, the team applied a Markov Process to a graded partially ordered set based on the clinical observations of COVID-19 cases to ascertain the most likely order of the symptoms in patients.
The team compared the progression of the COVID-19 symptoms to other respiratory illnesses, including the severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), and influenza. The team wanted to observe if the diseases have different manifestations.
The study model projects that influenza begins with a cough, while COVID-19, just like other coronavirus-related illnesses, starts with a fever. Further, COVID-19 is different from SARS and MERs in the order of gastrointestinal symptoms.
Fever and cough are frequently tied to many respiratory diseases, including MERS and SARS, but the timing and symptoms in the upper and lower gastrointestinal (GI) tract could set COVID-19 apart. For instance, the upper GI tract seems to be affected before the lower part in COVID-19, which is the opposite of the other two coronavirus relatives.
"The order of the symptoms matter. Knowing that each illness progresses differently means that doctors can identify sooner whether someone likely has COVID-19, or another illness, which can help them make better treatment decisions," Joseph Larsen, study lead author said.
The findings highlight the importance of checking for body temperature, not only in arrival sites or entry to facilities.
"Our results support the notion that fever should be used to screen for entry into facilities as regions begin to reopen after the outbreak of Spring 2020. Additionally, our findings suggest that good clinical practice should involve recording the order of symptom occurrence in COVID-19 and other diseases," the team said.
To slow the spread of COVID-19, the study findings underline the importance of testing fever before allowing people to enter the facilities. Also, contact tracing should be done to isolate the patients.