Over the past several months, the coronavirus pandemic has rippled worldwide, infecting more than 21.67 million people. Though new details about the novel coronavirus, now called the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), are slowly emerging, reports have shown that some people who were infected in the past contracted the virus again.
Questions have been raised by many health experts on whether being infected with SARS-CoV-2 brings lasting immunity. Now, scientists have uncovered signs of strong and lasting immunity in people who even had a mild illness of COVID-19.
The studies, which are not yet peer-reviewed and appeared on medRxiv*, have revealed that antibodies and immune cells that can fight off the virus are present in people who have been infected in the past, warding off the possibility of re-infection.
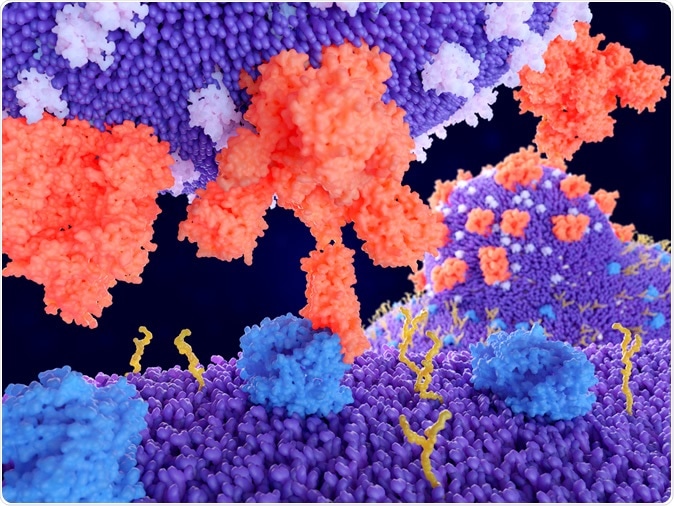
Binding of the coronavirus spike protein(red) to an ACE2 receptor (blue) on a human cell leads to the penetration of the virus in the cell, as depicted in the background. Illustration Credit: Juan Gaertner / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
What is immunity?
Immunity is the ability of the human body to resist a particular infection or toxin through the use of antibodies or sensitized white blood cells. Adaptive immunity happens after exposure to an antigen, such as a pathogen or a vaccination. It is triggered and stimulated when the innate immune response is insufficient to control infection.
The adaptive immunity response includes cells that produce targeted antibodies that can bind to the virus to kill it. From there, immune cells develop a memory of the specific antigen, and whenever the body re-encounters it, it can effectively kill it, reducing the risk of re-infection.
Other diseases, such as chickenpox, mumps, and measles, among others, trigger the adaptive immune system of the body. Hence, when a person contracts the viruses for these illnesses the second time around, the body is more capable of eradicating the infection.
The immune system’s memory may remember infections efficiently but may also forget others. For instance, people who had measles should have life-long immunity even with just one bout. However, some illnesses may recur, including common colds and the respiratory syncytial virus, which children contract many times even in the same winter season.
Currently, the SARS-CoV-2 has not been around long enough for scientists to determine if how long its immunity will last.
Persistent immunity
In the new studies, scientists have shown that SARS-CoV-2 infection could provide long-lasting immunity for those who were already infected. The first study, titled, “Evidence for sustained mucosal and systemic antibody responses to SARS-CoV-2 antigens in COVID-19 patients,” has shown that anti-SARS-CoV-2 antibody responses were detected in the blood and saliva of those who were infected with the virus, compared to those in the control group.
To arrive at their findings, the Canadian research team developed enzyme-linked immunosorbent assays to detect the presence of immunoglobulin A (IgA) and immunoglobulin B (IgB) antibodies to the SARS-CoV-2 spike protein and its receptor-binding domain (RBD) in the blood and saliva of acute and convalescent patients who were diagnosed with COVID-19.
The team also found that the antibodies were found with peak IgG levels achieved by 16 to 30 days post-symptom onset. Further, IgA antibodies rapidly degenerated, but the IgG antibodies persisted and remained stable up to 115 days post-symptom onset in both the blood and saliva samples.
“Importantly, IgG responses in saliva and serum were correlated, suggesting that antibodies in the saliva may serve as a surrogate measure of systemic immunity,” the team reported.
“Our findings that the IgG response to SARS-CoV-2 antigens is stable over 3 months are consistent with two other studies who likewise noted durability in the IgG response to the spike trimer,” they added.
The team concluded that the study provides evidence that that IgG response to the novel coronavirus persists in the saliva and blood.
“Given that SARS-CoV-2 initially replicates in the oro- and nasopharyngeal tracts, in the future it will be critical to characterize the nature and kinetics of salivary antibodies at the earliest time points post-infection in contact-traced individuals to determine if there are correlates of protection that impact viral setpoint and COVID-19 disease progression,” the team, who were from the University of Toronto in Canada, noted.
Immunity even after mild COVID-19
Another study published in medRxiv*, a team of researchers unveiled that functional SARS-CoV-2-specific immune memory persists even after developing even mild COVID-19.
In the study by researchers at the University of Washington in the United States, the team performed a longitudinal assessment of people who have recovered from mild COVID-19 infection to determine if they develop and sustain immunity against the virus.
The researchers found that those who recovered from SARS-CoV-2 infection developed specific IgG antibody and neutralizing plasma, as well as virus-specific memory B and T cells that persisted and even increased in number over three months following the onset of symptoms.
“Furthermore, the SARS-CoV-2-specific memory lymphocytes exhibited characteristics associated with potent antiviral immunity: memory T cells secreted IFN-γ and expanded upon antigen re-encounter, while memory B cells expressed receptors capable of neutralizing virus when expressed as antibodies,” the researchers wrote in the paper.
“These findings demonstrate that mild COVID-19 elicits memory lymphocytes that persist and display functional hallmarks associated with antiviral protective immunity,” they added.
Possible protective immunity
A third study, which has not been peer-reviewed and appeared on medRxiv*, has provided evidence that among people who developed symptomatic COVID-19, RBD-targeted antibodies can indicate previous and recent infection. Also, they found that IgG antibodies are tied to neutralizing antibodies and are possibly linked to protective immunity.
To arrive at the findings of the study, the team measures the kinetics of early antibody responses to the RBD of the spike protein of SARS-CoV-2 among 259 infected people with symptoms. They compared the antibody levels to more than 1,500 people whose blood samples were obtained before the emergence of the coronavirus pandemic.
They found that between 14 and 28 days from the onset of the symptoms, IgG, IgA, or IgM antibody responses to RBD were all accurate in determining recently infected people, with a 100 percent specificity and a sensitivity of 97 percent, 91 percent, and 81 percent, respectively.
IgA and IgM antibodies lasted shorted, with the infected people projected to become seronegative again by 51 and 47 days after the onset of symptoms, respectively. However, IgG antibodies persisted longer by 75 days of post-symptoms onset.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Sources:
- Rodda, L., Netland, J., Shehata, L., Pruner, K. et al. (2020). Functional SARS-CoV-2-specific immune memory persists after mild COVID-19. medRxiv. https://www.medrxiv.org/content/10.1101/2020.08.11.20171843v2
- Iyer, A., Jones, F., Nodoushani, A. et al. (2020). Dynamics and significance of the antibody response to SARS-CoV-2 infection. medRxiv. https://www.medrxiv.org/content/10.1101/2020.07.18.20155374v1
Journal references:
- Preliminary scientific report.
Isho, B., Abe, K., Zuo, M., Jamal, A., Rathod, B. et al. (2020). Evidence for sustained mucosal and systemic antibody responses to SARS-CoV-2 antigens in COVID-19 patients. medRxiv. https://www.medrxiv.org/content/10.1101/2020.08.01.20166553v1
- Peer reviewed and published scientific report.
Rodda, Lauren B., Jason Netland, Laila Shehata, Kurt B. Pruner, Peter A. Morawski, Christopher D. Thouvenel, Kennidy K. Takehara, et al. 2020. “Functional SARS-CoV-2-Specific Immune Memory Persists after Mild COVID-19.” Cell 184 (1). https://doi.org/10.1016/j.cell.2020.11.029. https://www.cell.com/cell/fulltext/S0092-8674(20)31565-8.