Eight months into the COVID-19 pandemic, it appears that women have a survival advantage over men concerning the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The question as to whether this could help develop better therapies requires that the physiological basis of this difference be unveiled. A new study published on the preprint server medRxiv* in August 2020 shows that the risk of infection is high for pre-menopausal women but the risk of death is much higher for men in the same age group and throws light on the protective nature of estradiol therapy in post-menopausal women.
It is known that SARS-CoV-2 infection can occur across all ages. However, the rate is higher among men, at about 60%, vs. 40% in women. Men are also far more likely to be critically ill with COVID-19, and two-thirds of all COVID-19-related deaths are in men. The infection also takes a higher toll in terms of fatality among older people over 60 years of age.
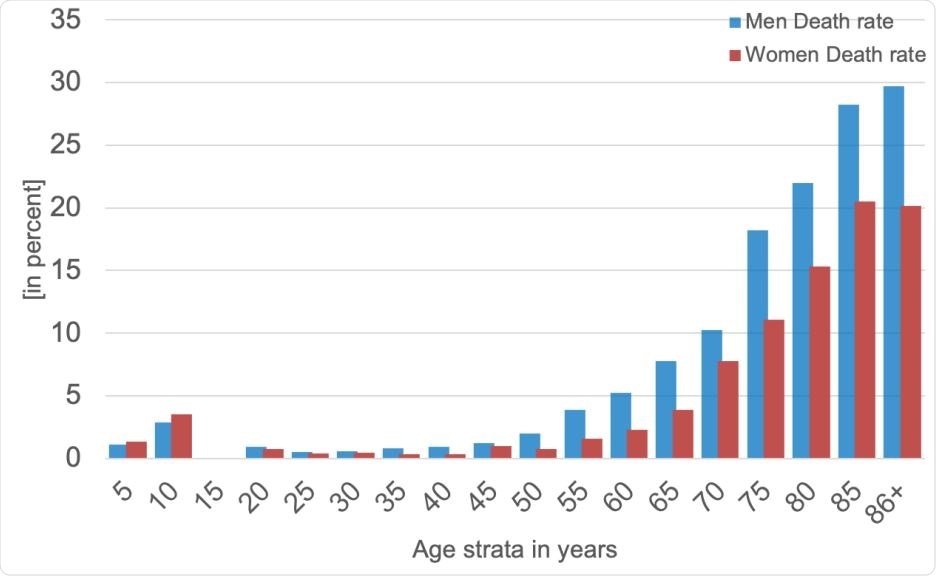
A histogram of death rates for women (red) and men (blue) in five-year age strata: 10 Cumulatively, men were more vulnerable to SARS-CoV-2 infection, with a fatality rate in some 11 strata that is roughly +50% higher than that in women.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Molecular Mechanism of Estradiol Protective Effects
The current study looked at the effects of systemic estradiol and infection rates. The researchers looked at the odds ratios for survival in over 37,000 women in two groups, one aged 15-49 years and the other over 50 years of age.
This virus uses the angiotensin-converting enzyme (ACE2) to enter the host cell. This receptor is found in a wide range of tissues. It takes part in the renin-angiotensin system (RAS), which regulates vascular and organ-protective functions, and is encoded on the X chromosome, which also houses the AT2 gene. Due to this location, it has a different expression in the two sexes.
Moreover, estradiol acts differently on various RAS components. For instance, it counter-regulates the classical angiotensin-converting 12 enzyme (ACE)/ angiotensin II (AngII)/ angiotensin II receptor type 1 (AT1R) signaling pathway.
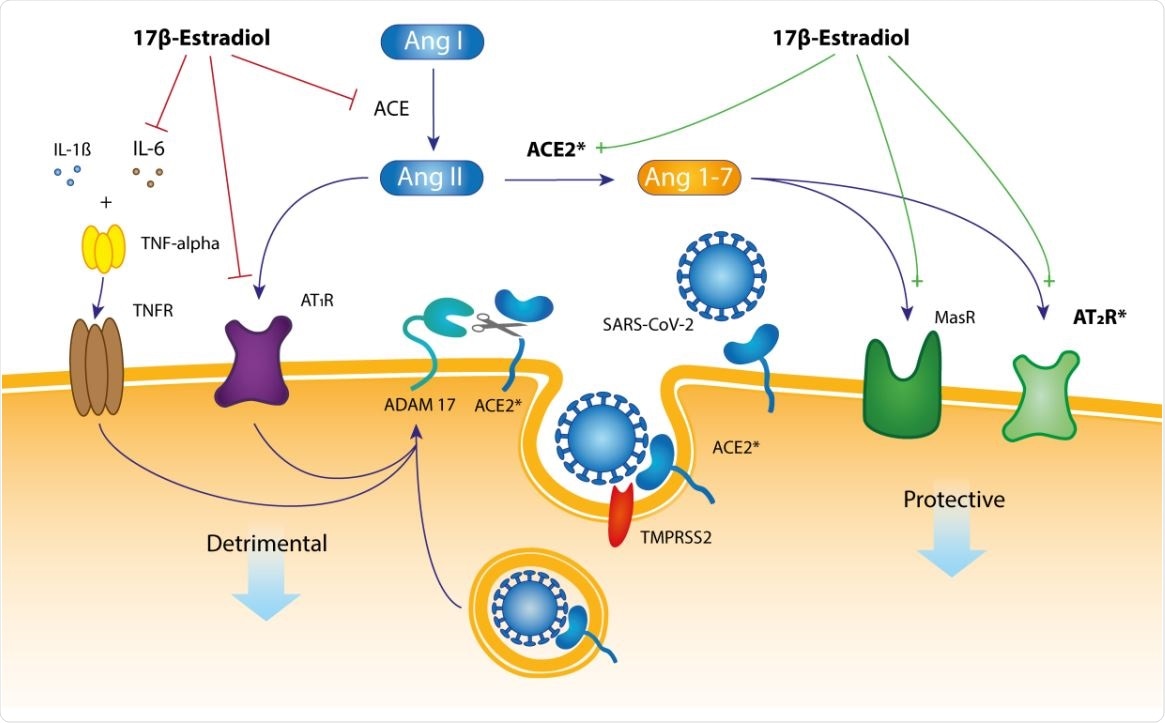
A hypothetical mechanistic pathway for the presumably protective role of 17β estradiol in SARS-CoV-2 infection. The membrane-tethered ACE2 protein has an amino terminal catalytic domain (a peptidase) that faces the extracellular space.
It could also act by activating the Mas receptor or AT2R, which in turn, inhibits fibrosis, has anti-oxidant, anti-hypertrophic, and vasodilatory effects. This could protect target cells and organs. It may thus mediate protective effects for target organs and tissues such as those of the lung, kidney, heart, cardiovascular system, adipose tissue, gut, testes, and the central nervous system.
Estrogen also downregulates IL-6, a cytokine that triggers inflammation in many tissues, while androgens upregulate it. “IL-6 is a cytokine with both anti- and pro-inflammatory effects. It can be produced by almost all stromal and immune system cells, and it is believed to play a central role in precipitating the cytokine storms 21 that, in turn, yield such severe symptoms from a SARS-CoV-2 infection,” say the researchers.
The researchers comment that by virtue of these multiple estrogen interactions, “While pre-menopausal women might be at a higher risk of initial SARS-13 CoV-2 infection, they are more protected from a severe course of the disease.”
Higher Infection, Lower Mortality, in Premenopausal Women
The researchers found that the highest infection in numerical terms is among women aged 15-49 years, about 15% higher compared to men of the same age. At this age, women would be expected to have the highest levels of serum estradiol. At 60-85 years, the frequency among women declines to that of men. However, the infection risk is similar in children of both sexes.
Men, however, have about 50% higher mortality rates following SARS-CoV-2 than women. In both sexes, there is an age-related increase in COVID-19 fatality rates, but at about 50 years, there is a sudden increase for men, to more than double the risk in women of that age. Survival at 200 days after diagnosis is also lower in men. While factors other than hormones may be at play, such as smoking or lifestyle patterns, intrinsic or physiological factors are also likely to be important.
The researchers explain some potential factors in this sex difference. Firstly, conditions like advancing age could cause a reduction in ACE2 expression. Secondly, it could cause a direct loss of active ACE2 receptors due to binding by the virus. Both of these might explain why men have a worse outcome. Estrogen also regulates inflammatory activity, and this could again affect the lung and vascular symptoms of COVID-19 in men and women differently.
Both peri- and post-menopausal women aged 50 years or more who regularly used estradiol had a survival rate of almost 97% at 180 days from diagnosis, compared to 85% for non-estradiol users. In this group, the odds of death were 67% lower in users, and the risk of death was 70% lower. This lower risk is not seen in pre-menopausal women, perhaps because they already have endogenous estradiol levels.
“This retrospective study of hormone therapy in female COVID-19 patients shows that the fatality risk for women >50 yrs receiving estradiol therapy is reduced by more than 50%.” While the higher infection rate may be due to higher basal levels of ACE2 in pre-menopausal women, the reduced fatality rate could be due to “the relative 6 dominance of the MasR- and AT2R-based receptor signaling pathways in pre-menopausal women [which] has positive (beneficial) impacts upon downstream organ function, with its attendant vascular protection and immunomodulatory effects."
This is the first study to examine how exogenous estradiol use affects COVID-19 fatality rates. Currently, trials on exogenous estrogen and testosterone are ongoing to assess the effect on COVID-19 outcomes. If successful, a transdermal 7-day estradiol patch could be used to supply estrogen and reduce symptom severity in men and post-menopausal women with the infection, before intubation is required. This may need more evaluation of how long estradiol must be given before it produces positive effects on the lung.
The study shows that estradiol replacement or contraceptives can be safely continued in this pandemic season, especially in post-menopausal women, since it reduces the mortality even if it increases the infection risk. The researchers suggest this points to the need for prospective studies on the role estrogen plays in protecting against infection.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources