Early in the coronavirus disease (COVID-19) pandemic, the disease was recognized as a respiratory illness. As the outbreak spread across the globe, infecting more than 24.35 million people, evidence showed that the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) also affected other vital organs and systems in the body.
Now, a new study by a team of researchers at the Mount Sinai Health System in New York has shown that blood thinners may reduce the risk of death by up to 50 percent among severely ill hospitalized COVID-19 patients.
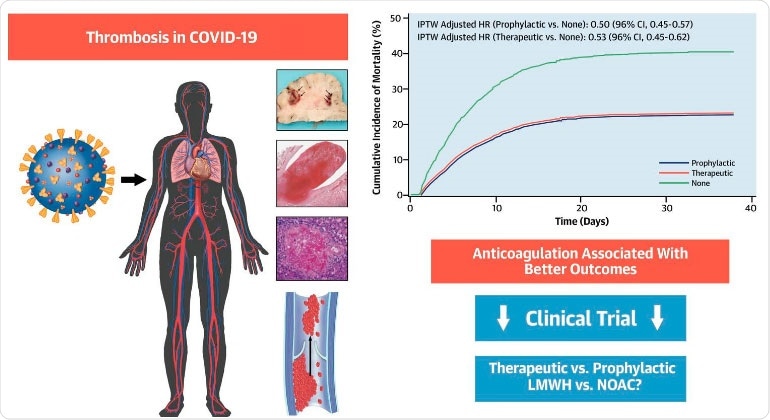
Thromboembolic disease is a complication of COVID-19. Prophylactic and therapeutic anticoagulation are associated with better outcomes in hospitalized patients with COVID-19. randomized controlled trials evaluating different AC regimens in COVID-19 are needed.
The study
The research team aimed to examine the link between anticoagulation with in-hospital outcomes and describe thromboembolic findings on patients' autopsies.
To arrive at the study findings, the team conducted a retrospective analysis to examine the link of anticoagulation with death, intubation, and significant bleeding. They analyzed the association of therapeutic versus prophylactic anticoagulation initiated within 48 hours from admission.
The team included all patients who were treated for less than 48 hours after admission with an anticoagulant. However, patients who stopped the drug due to significant bleeding were not included.
In the study, published in the Journal of the American College of Cardiology, among 4,389 patients, those with anticoagulation had lower in-hospital death and intubation. When the drug was given within 48 hours upon admission, there was no significant difference between therapeutic and prophylactic dose.
Further, in-hospital mortality risk was 50 percent lower with standard prophylactic dosing, and 47 percent lower with higher therapeutic-level dosing. Intubation was also less likely for COVID-19 patients treated with anticoagulants.
"Association of in-hospital anticoagulation (AC) was associated with lower mortality and intubation among hospitalized COVID-19 patients. Compared to prophylactic AC, therapeutic AC was associated with lower mortality, though not statistically significant. Autopsies revealed frequent thromboembolic disease. These data may inform trials to determine optimal AC regimens," the team concluded.
In a nutshell, 467 or 10.6 percent of the patients required intubation and mechanical ventilation during their hospital stay. Those on therapeutic blood thinners had 31 percent fewer intubations than those not taking blood thinners, while those on the prophylactic dose had 28 percent fewer intubations.
When the researchers examined the autopsies of some of the patients who died, about 42 percent had blood clots in their organs, such as the brain, lungs, liver, and heart.
"This work from the Mount Sinai COVID Informatics Center provides additional insight into the role of anticoagulation in the management of patients admitted to the hospital with COVID-19. Although this is an observational study, it helped in the design of a large-scale international clinical trial that we are coordinating. The randomized trial focuses on those three antithrombotic regimens -- therapeutic and prophylactic subcutaneous low-molecular-weight heparin, and therapeutic oral apixaban," Dr. Valentin Fuster, Director of Mount Sinai Heart and Physician-in-Chief of The Mount Sinai Hospital, said.
Though the study was not randomized controlled research, the researchers said that an international randomized trial just started with 15 institutions. They are comparing three types of anticoagulants that work.
Lung injury and blood clotting
Previous studies have shown that patients who have died from COVID-19, both had lung injury and signs of blood clotting in many organs.
In a study published in The Lancet: Microbe, the researchers report that their post-mortem study of patients who died from COVID-19 shows severe lung damage and signs of blood clotting in major organs. In the ten post-mortem examinations performed on patients who had COVID-19, revealed that all patients had lung injuries and early scarring of the lungs. They also had kidney injury.
Of these patients, nine had manifested thrombosis, a blood clot, in at least one major organ, including the lungs, heart, or kidneys.
"The UK has sadly had a large number of deaths related to COVID-19. The search for effective treatments will rely on an understanding of how the disease affects the body. The post-mortem examination is vital in this respect," Dr. Brian Hanley, from the Department of Cellular Pathology at Imperial College Healthcare NHS Trust, said.
"The findings in this study support research from other autopsy groups worldwide and in the UK that describe the structural damage to organs caused by COVID-19. It also documents several unexpected complications. This increased understanding of COVID-19 can help clinical teams with the management of severe cases and also to monitor and treat further complications as a result of the disease," he added.
Source:
Journal references:
- Anticoagulation, Mortality, Bleeding and Pathology Among Patients Hospitalized with COVID-19: A Single Health System Study, Girish N. Nadkarni, Anuradha Lala, Emilia Bagiella, Helena L. Chang, Pedro Moreno, Elisabet Pujadas, Varun Arvind, Sonali Bose, Alexander W. Charney, Martin D. Chen, Carlos Cordon-Cardo, Andrew S. Dunn, Michael E. Farkouh, Benjamin Glicksberg, Arash Kia, Roopa Kohli-Seth, Matthew A. Levin, Prem Timsina, Shan Zhao, Zahi A. Fayad, Valentin Fuster, J Am Coll Cardiol. 2020 Aug 26. Epublished DOI:10.1016/j.jacc.2020.08.041https://www.onlinejacc.org/content/early/2020/08/24/j.jacc.2020.08.041
- Hanley, B., Naresh, K., Roufosse, C., et al. (2020). Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: a post-mortem study. The Lancet: Microbe. https://www.thelancet.com/journals/lanmic/article/PIIS2666-5247(20)30115-4/fulltext