A recent observational study by US researchers reveals that individuals with non-alcoholic fatty liver disease and steatohepatitis have increased odds of hospitalization due to coronavirus disease (COVID-19); conversely, metabolic surgery was found to be protective against the admission of infected individuals. The study is currently available on the medRxiv* preprint server.
Fatty liver, liver steatosis, 3D illustration, and photomicrograph showing large vacuoles of triglyceride fat accumulated inside liver cells, it occurs in alcohol overuse, under action of toxins. Image Credit: Kateryna Kon / Shutterstock
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread around the globe since it first emerged in December 2019 in China, causing more than 26.2 million cases and over 866,000 deaths as of September 4, 2020.
Albeit there is still a lot to learn about this novel pathogen, as the information about the virus and the resulting disease (COVID-19) is evolving rapidly. We already know the most critical risk groups for severe clinical presentations, such as the elderly, those living with diabetes, and those with other chronic conditions (such as heart and lung disease).
Hepatic steatosis (comprising non-alcoholic fatty liver disease and non-alcohol steatohepatitis) correlates well with visceral adiposity, developed metabolic disease, as well as overt and chronic inflammation process.
Taking into account that COVID-19's pathophysiology is tightly linked to inflammation, non-alcoholic fatty liver disease and steatohepatitis may also represent significant risk factors that put patients with the disease at higher risk of poor disease outcomes; nonetheless, the research on this (and possible mitigating factors) has been scarce.
This is why researchers from the University of Minnesota, University of Miami, and Johns Hopkins School of Medicine sought to appraise the risk of hospitalization for COVID-19 associated with non-alcoholic fatty liver disease and steatohepatitis.
An observational in-depth appraisal
In short, this study represents the first in-depth assessment of hepatic steatosis as a risk factor for hospital admission of COVID-19 by analyzing an extensive database in the United States, as well as possible treatments for avoiding this scenario.
A retrospective analysis of electronic medical records from 56 primary care clinics and 12 hospitals has been pursued. More specifically, over 6,700 adults with positive SARS-CoV-2 test results were included between March 1, 2020, and August 25, 2020.
A primary objective was a precise quantification of hospitalization risk for COVID-19 based on the history of non-alcoholic fatty liver disease and steatohepatitis. Furthermore, the researchers also wanted to see how known treatments for metabolic disease modified this risk, as well as if there any gender or racial differences.
Increased hospitalization risk
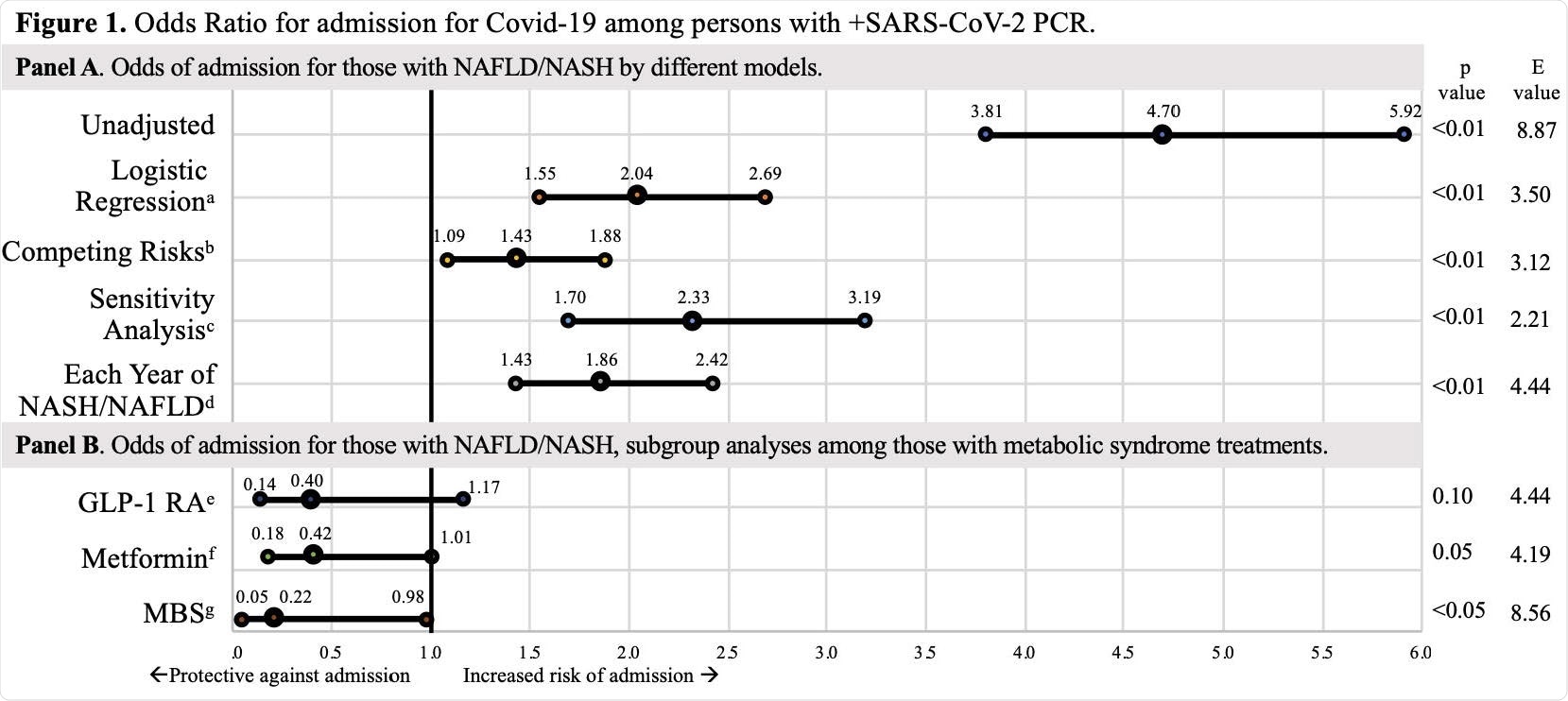
In a nutshell, this study has shown that the medical history of hepatic steatosis was associated with increased odds of admission to hospital due to COVID-19. Each additional year of having either non-alcoholic fatty liver disease or steatohepatitis was also linked to a significantly increased risk of being hospitalized for COVID-19.
When demographic characteristics were appraised, it was revealed that hepatic steatosis increased the risk of hospitalization in both men and women, and significantly elevated the same risk within each racial subgroup – with the largest rise seen among individuals who self-identified as black.
"Promisingly, we found that known treatments for metabolic syndrome and NAFLD/NASH greatly mitigated risks from COVID-19 – those with home metformin or glucagon-like peptide-1 receptor agonists use had a nonsignificantly reduced odds of hospitalization, and those who had undergone bariatric surgery had a significant decrease in odds of hospitalization", further say researchers.
Treatment implications
"Non-alcoholic fatty liver disease/steatohepatitis is a state of chronic inflammation due to visceral adiposity, is a significant risk factor for hospitalization for COVID-19, and appears to account for risk attributed to obesity", summarize study authors in this medRxiv study.
Of course, more research is needed to verify these findings. Still, patients with elevated body mass index can already be screened for hepatic steatosis and informed of all the risks associated with visceral adiposity and COVID-19, as well as opportunities as mentioned above to mitigate it.
And while the protective benefits of metformin, glucagon-like peptide-1 receptor agonists, and bariatric surgery are promising, more treatment options for non-alcoholic fatty liver disease/steatohepatitis are urgently needed.
Weight loss is still the mainstay of treatment, and while breakthroughs in obesity medicine have enabled a sustainable approach to it, societal forces (including the ongoing pandemic) continue to foster an obesogenic environment. This is something further research endeavors also need to address specifically.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.