The COVID-19 pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is still spreading across many parts of the world, and clinicians are working on recognizing biomarkers that are of value in predicting the risk of mortality in each case so as to make appropriate clinical decisions. This is also necessary for designing clinical studies and assessing the outcome of various novel treatments. Now, a new study published on the preprint server medRxiv* reports the use of D-dimer in predicting the risk of mortality in COVID-19.
At present, there is little evidence to show which patients are at the most significant risk of dying. For this reason, a general clinical profile is used to make the necessary decisions. This includes laboratory test results and examination findings.
D-dimer in COVID-19
The researchers evaluated the role of D-dimer, a fragment of protein produced by the break-up of fibrin clots that are typically linked to each other. This is a biomarker of importance in suspected thromboembolism (VTE). Some recent research demonstrates that when a patient with COVID-19 has high D-dimer levels when admitted in hospital, the risk of death is elevated.
The role played by D-dimer relates to the high procoagulable state in COVID-19, as shown by the remarkable decline in mortality when those with high D-dimer levels are treated with anticoagulation. As a result, anticoagulants are now recommended in many protocols and guidelines, either using full doses for therapeutic use or intermediate doses for prophylactic use, to prevent thrombotic events in patients with severe COVID-19 infection and especially when D-dimer levels are high.
The current study focuses on evolving monitoring and interpretation standards for D-dimer levels in hospitalized patients. The basic premise to be tested was that the mortality risk could be predicted using baseline and changing D-dimer levels, in combination with other risk factors.
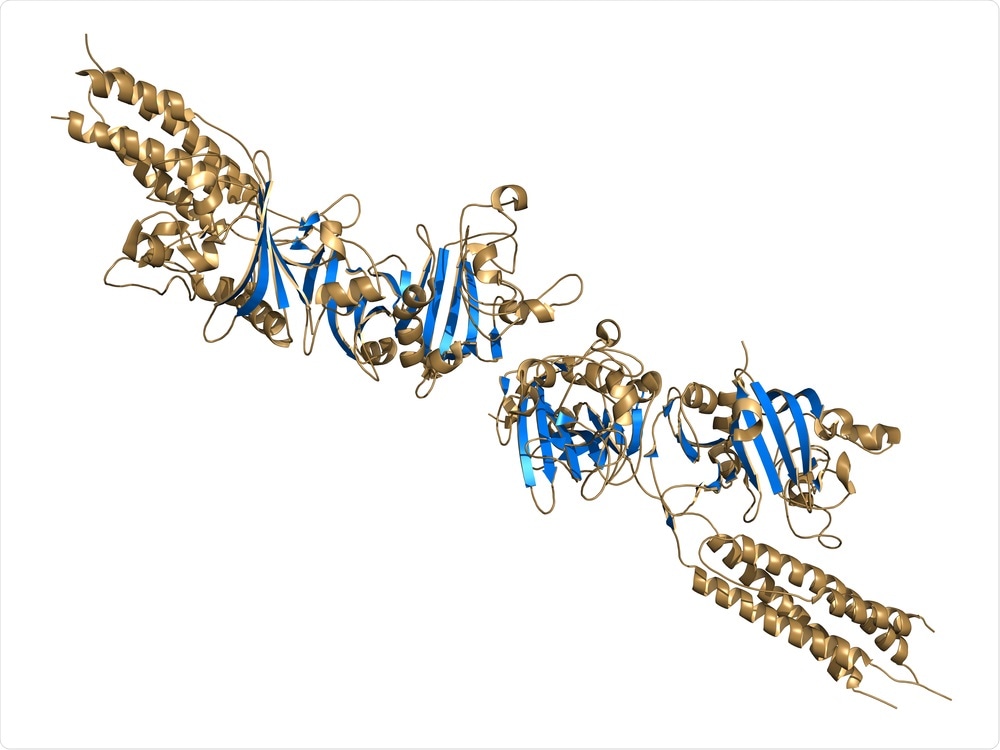
D-dimer fibrin degradation product, chemical structure. When found in the blood, D-dimers are indicative of the presence of blood clots (thrombosis). Image Credit: StudioMolekuul / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Anticoagulation in COVID-19
The researchers from the Icahn School of Medicine at Mount Sinai exploited a large patient dataset, using records from the Mount Sinai Health System (MSHS) in New York City. This gave them access to baseline sociodemographic data, risk factors like coexisting illnesses, body mass index (BMI), and the presence of smoking. The most abnormal recordings of several vital signs at the point of admission were also retrieved, including the temperature, heart rate, respiratory rate, blood pressure, and oxygen saturation. So were the early laboratory tests sent within 24 hours of admission and before beginning anticoagulant prophylaxis or therapy.
There were over 1,800 adult patients, with a median age of 67 years, about 60% being males, who were on therapeutic anticoagulation during their hospital stay. Almost three-quarters of them were discharged, while the rest did not survive.
The MSHS protocol for anticoagulant therapy was implemented for hospitalized COVID-19 patients, provided they had no increased risk of bleeding. Therapeutic doses were given to all patients whose assessment showed a risk of or the presence of VTE, or for those with severely impaired breathing. For others, prophylactic doses were started. The drugs used were heparin, enoxaparin and/or apixaban.
D-dimer Levels at Admission and Mortality Risk
The D-dimer level was used to classify them into four cohorts – the determinants being the initial concentration and the direction of change with anticoagulation.
The first was the high-increase (HI) group with a high baseline level, which went up following treatment. The mortality rate in hospital for this cohort was 49%.
The second was the high-decrease (HD) group at 27% mortality. The third, or low-increase (LI), group and the last, or low-decrease (LD) group, had a mortality of 21% and 9%, respectively.
Patients with advanced age, multiple illnesses, more significant breathing impairment, worse kidney function, and signs of inflammation were generally at a higher risk of death during hospitalization and tended to have a longer delay from the start of the hospital period to the institution of anticoagulant therapy.
D-dimer Levels Post-Anticoagulation and Mortality Risk
After anticoagulation was provided, the subsequent levels of D-dimer showed higher levels for those patients who died vs. were discharged, with the median concentrations being 3.70 ug/ml and 1.70 ug/ml, respectively. These two groups (died vs. discharged) had a smaller gap at admission, in fact, at 2.02 ug/ml vs. 0.39 ug/ml, respectively.
Again, D-dimer levels were found to rise after anticoagulation for those who died in hospital, but to decline for those who were discharged. Thus, it was markedly easier to predict the risk of in-hospital death using an anticoagulant D-dimer level than the baseline D-dimer level. Using a combination of the two did not improve the predictive value further.
The patient cohort with high D-dimer levels after anticoagulation overlapped with the groups of patients who were older and sicker, with worse respiratory parameters at admission, and signs of more severe disease as marked by increased white cells but lymphopenia, renal disease and elevated inflammatory markers. Overall, there were ten factors significantly associated with a higher mortality rate.
Reliable Predictive Values
The researchers then looked at how the individual predictive factors in this model worked by leaving them out one by one and examining the impact. They found that age was most closely related to risk of mortality, but that the HD post-anticoagulant D-dimer group was close behind, followed by the HI post-anticoagulant D-dimer group and the platelet count, oxygen saturation and the LI post-anticoagulant D-dimer group.
The predictive power was highest with the classification by D-dimer level following anticoagulation, combined with selected baseline variables, and significantly better than that of baseline models alone.
Thus, the study on patients hospitalized with severe COVID-19 shows the “high and independent predictive power of post-anticoagulant D-dimer levels for in-hospital mortality, while taking into consideration 65 other important covariates.” The researchers also found the direction of change in D-dimer levels to be important in predicting mortality after anticoagulation. In fact, this is the single most crucial variable among all those examined in the current paper. This demonstrates that “post-anticoagulant D-dimer levels and trends are novel prognostic biomarkers that should be considered in the management of hospitalized COVID-19 patients.”
This conclusion differs from that of earlier studies showing high D-dimer levels to be markers of poor prognosis in COVID-19 patients when measured at the time of admission. In this study, the post-anticoagulant D-dimer was a reliable and sensitive indicator of mortality risk but not the point-of-admission D-dimer. In fact, the trajectory of the D-dimer was an important marker, since the LI group had higher mortality than the HD group.
The researchers consider more studies to be critical to improving the accuracy of prediction, using serial measurements to capture the changes in this parameter. If the level remains high or rises even after anticoagulation therapy, it may indicate that the risk of clotting is high in large vessels or the microvasculature.
Implications and Future Directions
The applications of this study are threefold:
First, this biomarker can be used to clarify treatment decisions by being made part of the therapeutic protocols for severe COVID-19. Since this was an observational study, confounding factors may have altered the outcome. To validate these findings, randomized controlled trials will be needed. In the long interim period, meanwhile, these outcomes will be of use in guiding the immediate management of hospitalized COVID-19 patients.
Secondly, the study shows that post-anticoagulation, the HI group is a subset of patients with a very poor outcome. The possibility of identifying this early will facilitate proper care and guide future studies on the treatment of this condition with antiplatelet drugs or thrombolytics.
Thirdly, it focuses attention on the patients at least risk, namely, the LD group, who will need to be analyzed further to reduce the dose of anticoagulation therapies, possibly as well as to understand if these drugs need to be continued further after their discharge.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Song, X. et al. (2020). Post-Anticoagulant D-dimer as a Highly Prognostic Biomarker of COVID-19 Mortality. medRxiv preprint. doi: https://doi.org/10.1101/2020.09.02.20180984. https://www.medrxiv.org/content/10.1101/2020.09.02.20180984v1
- Peer reviewed and published scientific report.
Song, Xiaoyu, Jiayi Ji, Boris Reva, Himanshu Joshi, Anna Pamela Calinawan, Madhu Mazumdar, Juan P. Wisnivesky, Emanuela Taioli, Pei Wang, and Rajwanth R. Veluswamy. 2021. “Post-Anticoagulant D-Dimer Is a Highly Prognostic Biomarker of COVID-19 Mortality.” ERJ Open Research 7 (3). https://doi.org/10.1183/23120541.00018-2021, https://openres.ersjournals.com/content/7/3/00018-2021