At its onset, the COVID-19 pandemic shocked the world, with the number of new cases and deaths growing more than 20% per day in the main hotspots. With a growth rate this high, the disease was expected to spread through the population in less than six months without mitigation, and to reach a peak after three months, at which point 30% of the population would have had the disease. This, however, was not how the initial wave of the epidemic played out. So far, the COVID-19 pandemic has been characterized by an initial rapid rise in new cases followed by a peak and more erratic behavior that varies between regions.
Early in the pandemic, scientists have observed that the spread of the virus is faster and more rampant in densely populated areas, where a large number of people congregate. The new study, which was published in the open-source medRxiv* and has not yet been peer-reviewed, shows that superspreaders and population heterogeneity are the core factors explaining the discrepancy of cases.
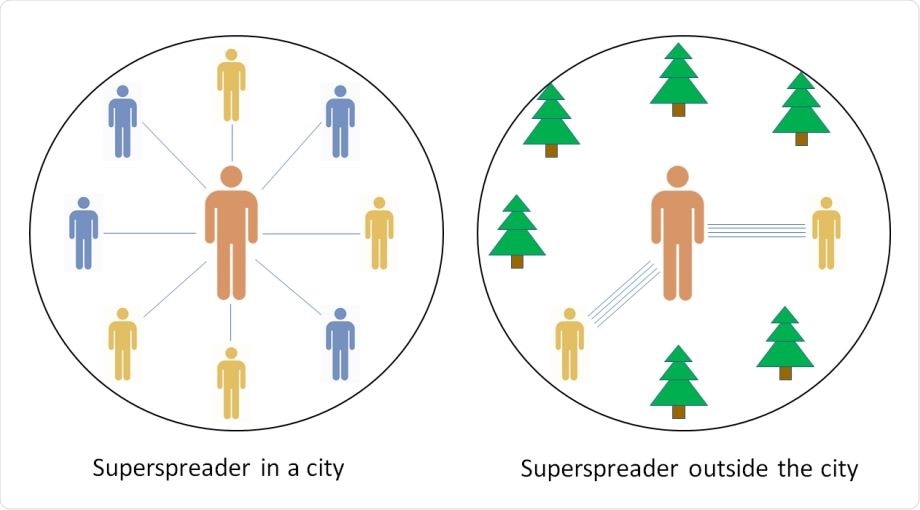
Model: A superspreader in a city interacts a little with a lot of people and will infect some fraction of them. On the other hand, a superspreader outside the city will interact a lot with each of a smaller set of people. The superspreader then infects practically all of them, but there is a lower cap on the number of secondary infections.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The study
In the study, the researchers noted that a rapidly spreading epidemic occurs in crowded areas. However, in less densely populated areas, the outbreak onset is delayed, and in rural areas, it never starts, with most cases appearing to be spillover from the cities.
The team proposed an agent-based lattice model of an infectious disease that spreads in a geographically heterogeneous population. The novel model is a simpler version of the dynamics of COVID-19, and it will help the team study the effect of the heterogeneous infection pattern.
The team compared superspreaders in cities with those in the countryside or less populated areas. They found that a superspreader in the city interacts with many people and will infect some fraction of them. Meanwhile, a ‘super spreader’ outside the city or in the countryside will interact with a lot with each of a smaller set of people. The infected person may spread the virus to all of the people, but there is a lower cap on the number of secondary infections.
“Thus, people in the countryside interact with a smaller set of people while still spending the same amount of time on social activities,” the team explained.
“From a wider perspective, this proposes that density dependence of disease spreading is more due to the difference in diversity of contacts than due to differences in time spent around other people. Thereby our model assumes an infection rate that depends on density, but not in a simple linear fashion as sometimes assumed,” they added.
The researchers noted that with no superspreaders, the epidemic or outbreak would spread unchecked in the countryside. Still, it will be slower because, in these areas, the space is geographically large than in the city.
The density of countryside areas
There are the delayed onset and unusual behavior of epidemics in the countryside, which depends on the density and other factors of the area. Also, the traveling pattern of people may have something to do with how an outbreak spreads in a particular area, such as cities and the countryside.
Put simply, in contrast to conventional disease models, the team believes that everyone is equally social, but the set of available contacts is smaller in less densely populated areas. When the density is lower, the groups that spend time with will be less diverse.
Further, the number of potential close contacts for each person ‘declines linearly with population density’. However, those who live in sparsely populated areas are more likely to have multiple encounters with the same people, as the communities are smaller.
Yet, superspreaders can transmit the virus even during short encounters. The length of time of each encounter becomes less critical, since even a brief encounter with a superspreader may lead to infection. Those infected people who interact with only a small number of people may limit secondary infections.
“Our study compounds this finding and suggests that a change in behavior is not strictly necessary to cause an epidemic peak well before herd immunity has been achieved. Mitigation strategies that primarily target cities may well be sufficiently effective in bringing down the epidemic,” the team concluded.
The team emphasized that large gatherings, such as weddings and funerals, were not included in the study. Public events like these may lead to the rapid spread of the virus, especially if there are no infection control measures.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Source:
Journal references: