COVID-19 is a zoonotic disease originated by SARS-CoV-2, thought to have been transferred from certain wild mammalian species to humans via an intermediate host. It is characterized chiefly by lung injury, with features similar to the macrophage activation syndrome that results in hyperinflammation, including the activation and proliferation of T cells and macrophages.
While there are several types of coronavirus, they fall into four genera, from alpha to delta. The two severe respiratory coronaviruses of earlier decades, namely, the SARS-CoV and MERS-CoV, are both betacoronaviruses (betaCoV), and both cause fatal pneumonia with a prominent inflammatory component. While immunocompetent people show mild infection, older adults and immunocompromised individuals are at risk for severe infection.
Dogs and cats have been found to be susceptible to alpha and betaCoV, for instance, the canine enteric coronavirus (CCoV), which causes gastroenteritis in animals. Some of these infected dogs recover to become carriers. The spread of CCoV occurs via the feco-oral route.
A betaCoV called canine respiratory coronavirus (CRCoV) causes mild respiratory infection in dogs. However, recently asymptomatic SARS-CoV-2 infection has been described for the first time in dogs. It seems plausible that the virus could jump from humans to dogs since it is a zoonotic disease in the first place.
Other Animals Infected with SARS-CoV-2
Many other animal infections have been reported, including cats, dogs, tigers, lions, minks, and ferrets. Ferrets and cats have been shown to be relatively sensitive to SARS-CoV-2, unlike fruit bats, dogs and hamsters. A human-animal-human pattern is postulated, with the first part of the chain being confirmed by the World Organization for Animal Health-OIE, but not the second. The authors point out, “To date, no cases of transmission from domestic or captive wild animals to humans have been described.” This ignores, however, the possibility that two mink farmworkers reported positive acquired the infection from the mink.
Seropositivity in Pet Dogs
Some studies show that pet dogs with SARS-CoV-2-positive owners are seronegative, but others have described both RT PCR-positivity and the presence of neutralizing antibodies against SARS-CoV-2 in dogs. As of now, 10 PCR-positive dogs have been reported worldwide, all belonging to homes with virus-positive owners, and more than half of them being symptomatic. Two PCR-negative dogs have been observed to be seropositive, one being asymptomatic and the other showing respiratory issues.
A large study of 3,500 pet dogs, cats, and horses in the US and Korea failed to show a single positive animal, however. This conclusion was also reached in France and Italy, with the latter study, covering ~800 animals, finding no PCR-positives but 19 seropositive animals with neutralizing antibodies.
Unexplained Intractable Respiratory Disease in Dogs
The current study shows that serious respiratory disease was much increased among pet dogs, as reported by Spanish veterinarians, in a period overlapping the months of COVID-19 in Spain. The study aimed to describe the disease process in infected animals with COVID-19-like symptoms and to find out if dogs can acquire the virus in a home environment in close contact with humans.
The study included 40 sick dogs, with an average age of 8 years, belonging to 15 breeds. There were also 20 healthy dogs living in families with COVID-19. Most sick dogs had positive lung signs, but some also had a fever, a rapid pulse, and gut symptoms.
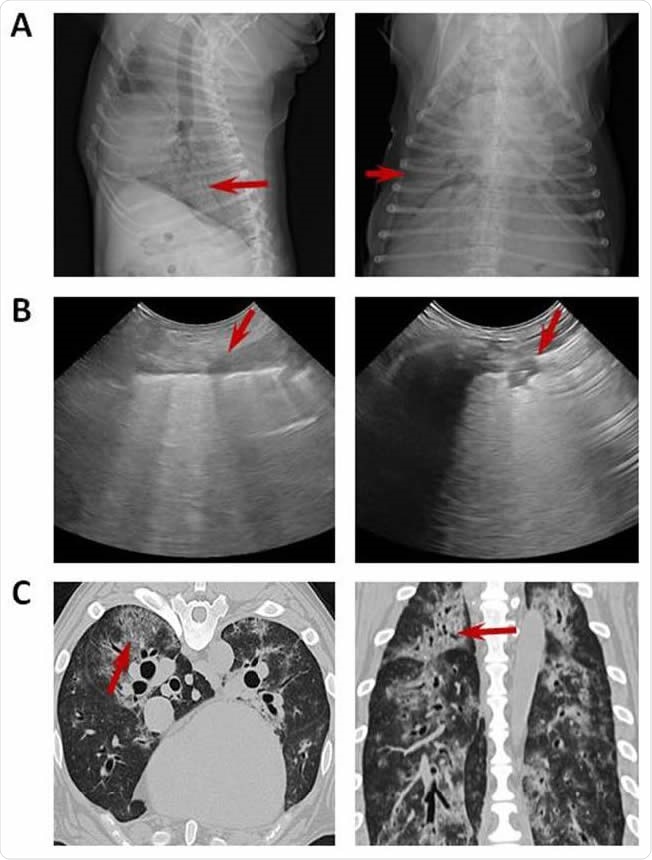
Imaging with chest radiograph, sonographic images and CT. (A) Thoracic radiograph made in right lateral (left) and dorsoventral (right) showing a generalized severe interstitial opacity accentuated in the caudodorsal (arrows). (B) Sonographic images of two patients with severe dyspnea showing a diffused B line (left; arrow) and consolidation focal lesions (right; arrow). (C) Transverse (left) chest CT images showing bilateral focal peripheral ground-glass opacities with intralobular and interlobular smooth septal thickening (arrow); sagital (right) chest CT images showing diffuse opacities with consolidation and bronchial wall thickening (arrow).

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
All sick dogs had radiological signs of alveolar or interstitial pneumonia. In over a third, generalized lung opacity was present, and in half, a single alveolar focus of infiltration. Ultrasound and CT scans showed bilateral parenchymal abnormalities.
A blood count was determined, which showed that in almost 60% of dogs, white cells were abnormally increased, mostly neutrophils but also monocytes in half and lymphocytes in over a third. They also screened for SARS-CoV-2, and 33 were also tested for other common canine viruses. All tests were negative, but one dog had CDV positive tests, with a third being reported Mycoplasma positive.
Respiratory disease in dogs is typically mild, but in this study, just less than half of the dogs died of their pneumonia during the follow-up. Necropsies in two dogs showed severe interstitial pneumonia with diffuse alveolar damage. The changes reflected those seen in viral infections of the lung.
Antibody Responses
The study next explored the immune responses in 17 sick dogs and 20 asymptomatic dogs that lived with COVID-19-positive owners. Ten and eight sick dogs have been vaccinated according to the standard protocol they failed to find any link between canine vaccination and the chances of subsequent sickness.
The researchers tested for IgG against the various canine viruses: canine adenovirus (CAV), canine parvovirus (CPV) and canine distemper virus (CDV), along with IgM and IgG isotypes against CCoV and IgG against SARS-CoV-2 in both groups. They found the last to be higher in a quarter of healthy dogs (5/17) but only one sick dog, which was, moreover, PCR-negative. This dog did show the presence of Mycoplasma spp. and CDV.
All of the five SARS-CoV-2 seropositive healthy dogs also had IgG antibodies against the first three canine viruses as well, but only two against CCoV. Vice versa, of the 12 healthy dogs, all were positive for CCoV IgG but only two for SARS-CoV-2 IgG. Of the seven sick dogs, none were seropositive for SARS-CoV-2.
Seropositivity and High Mortality in Dogs
Despite the scattered reports of seropositivity for SARS-CoV-2 in dogs, they are generally considered to be less susceptible to the virus. Yet, vets in Spain have reported a considerable jump in severe lung disease during the COVID-19 outbreak. Almost a third of US vets say that they were asked to diagnose COVID-19 in pet dogs during this time.
Most of the dogs in the Spanish report failed to respond well to the usual antibiotics. The expected mortality from respiratory disease in pet dogs is 1.2%, pneumonia accounting for only 0.3%. In the COVID-19 season, however, over 40% of dogs died due to respiratory disease.
Unknown Etiology
Though the etiological agent was mostly unidentified, they had severe lung disease similar to that seen in human COVID-19 pneumonia. Infectious respiratory diseases in dogs are typically due to CPIV, CAV-2, Bordetella bronchiseptica, Streptococcus equi subsp. zooepidemicus, Mycoplasma cynos, CHV-1, CDV, CIV, and CRCoV.
In the current study, 8/33 tested dogs showed signs of one of these pathogens, and CCoV in 3/17 sick dogs. However, CRCoV usually causes mild symptoms and signs and is unlikely to have been the cause of these acute severe lung disease episodes.
Mycoplasma was found in 26/33 dogs tested for a panel of organisms. The only species that is linked to canine pneumonia is M. cynos, but there is still doubt as to its actual pathogenic role. In most cases, it seems to be a coinfection or secondary infection. It is commonly identified in COVID-19 patients, and active Mycoplasma infection may steer the patient towards a fatal termination of the disease.
The 30-fold rise in the death rate among pet dogs, without an identifiable agent, is a curiously coincidental event in the COVID-19 period. While interstitial pneumonia is also seen in other dog diseases like canine distemper, septicemia, or herbicide exposure, in these dogs, it closely resembled the findings found in COVID-19 in humans. Further work is needed to examine this possibility given the negative PCR tests in nasopharyngeal and rectal samples.
In contrast to a Chinese study of ~500 dogs, where only one pet dog was seropositive, an Italian study on ~200 and ~60 dogs and cats showed the presence of neutralizing antibodies in about 3% and 4%, respectively. None were symptomatic.
Infected Owners Increase Chances of Canine Seroconversion
Dogs whose owners have COVID-19, or live in such households, have a higher chance of being seropositive. On the other hand, seroconversion occurs only in half the dogs that were exposed to the virus by seroconversion. The Italian study shows that about 13% of seropositive dogs came from infected households but only 1.5% from COVID-19-negative households. This information was not available in the current study.
Overall, therefore, the study concludes that of the 40 sick dogs, all were PCR-positive, but some were seropositive. Some healthy dogs also show seropositivity, suggesting a low level of transmission from dogs. Dogs belonging to infected owners are, however, likely to have higher levels of exposure to the virus.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources