Nine months into the COVID-19 pandemic much is still coming to light about the clinical features of the disease. Known for the high variability of its clinical severity, COVID-19 appears to behave differently in various clinical settings.
A new study by researchers at the University of California San Diego and published on the preprint server medRxiv* shows the occurrence of ocular pathology in the period of recovery following COVID-19. This throws more light on the occurrence of inflammation in people recovering from COVID-19.
Using Ocular Tomography to Identify Signs of Inflammation
The study included 15 people who had COVID-19 but had no recorded history of uveitis, inflammation of the pigmented tissues of the eye. The researchers used spectral-domain optical coherence tomography (SD-OCT), an imaging method capable of visualizing individual cells within the vitreous cavity. The vitreous is a part of the body that is separated from immunological processes due to the absence of direct blood supply.
Complete vs. Incomplete Recovery
The study included nine men and six women, of whom 14 had previously received a diagnosis of acute severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection by polymerase chain reaction (PCR) testing 58 to 85 days before the study began. The one exception had symptoms of COVID-19 and a confirmed case in the same household at the same time. All patients had respiratory symptoms, but only one required hospitalization.
All were in recovery according to accepted criteria, with a median of 50 days since recovery began. When asked about their subjective perception regarding the completeness of their recovery, 11 answered affirmatively at a median of 50 days from the beginning of recovery.
However, four indicated that they still had COVID-19-related symptoms at a median of 47 days from recovery. During this phase, four had a cough, two had weakness and numbness of the legs, while one developed sensitivity to light, and another had headaches.
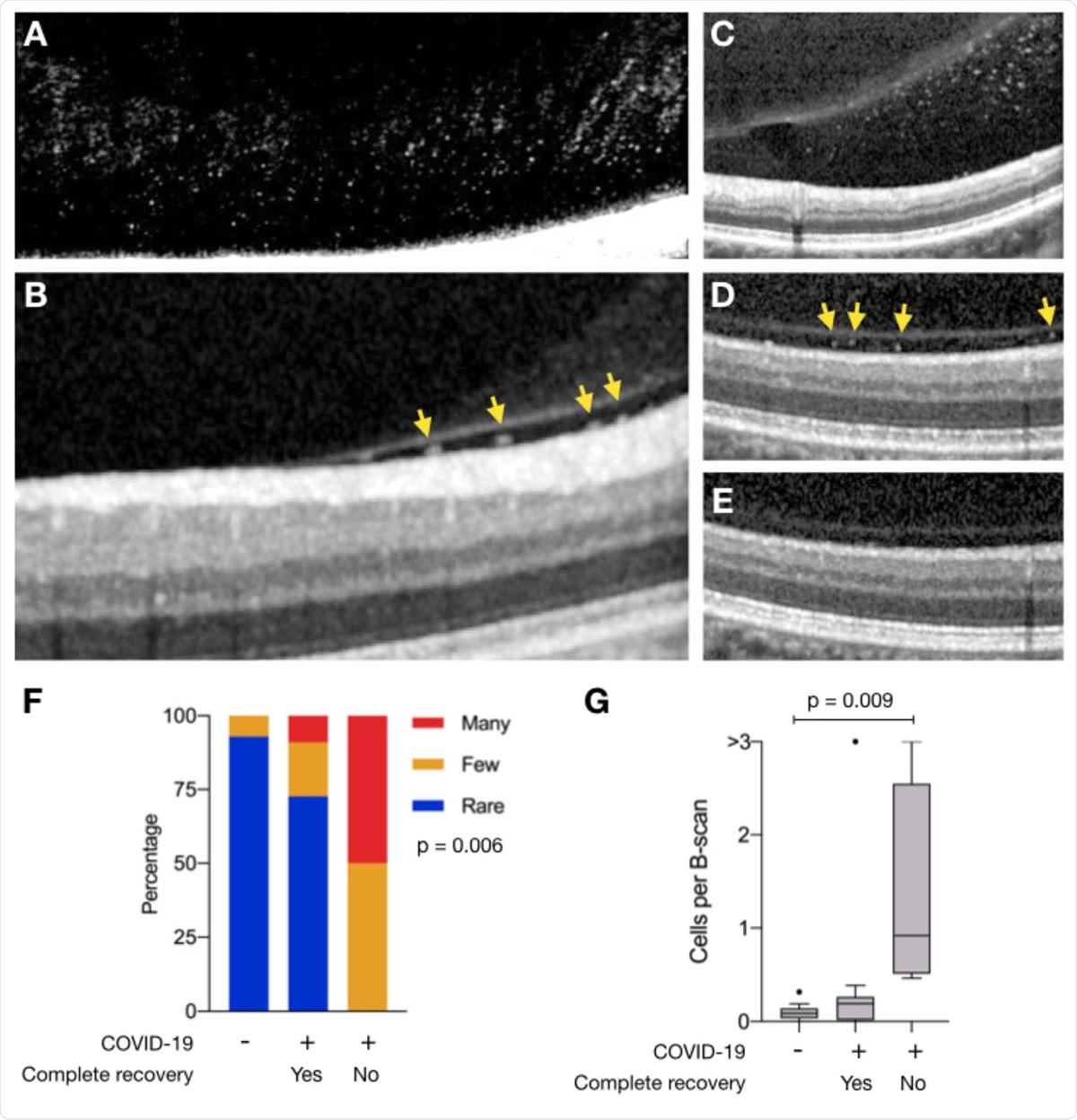
Vitreous cells in persons recovered from COVID-19. SD-OCT transverse sections of A) the posterior vitreous near the inferior macular vascular vessels in Participant 1 with many vitreous cells, B) the retina vitreous interface demonstrating cells (yellow arrows) in the sub-hyaloid space in Participant 5 and C) Participant 4. Identical SD-OCT transverse sections of the retina and vitreous of the right eye demonstrating many cells in the subhyaloid space after recovering from COVID-19 (D), and no vitreous cells 2 years prior (E). Corresponding infrared en face images of the retina (not shown) were used to determine the exact reference location. The image in panel A was digitally enhanced to highlight vitreous cells. The adjustment has been made to the entire image. (F) The distribution of vitreous cells grading (rare, blue; few, orange; many, red) among individuals with no history of COVID-19, and those with prior COVID-19 infection who fully recovered (Yes) and those who did not (No). Significance was determined using Pearson’s chi-squared test (p = 0.006). (G) Box plots showing the number of vitreous cells per transverse B-scans among individuals with no history of COVID-19, and those with prior COVID-19 infection who fully recovered (Yes) and those who did not (No). Significance was determined using one-way ANOVA (p = 0.01) and student’s test with Tukey’s correction.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Cellular Content of Vitreous Humor
The convalescents in the study had SC-OCT scans, and the B scans were examined to analyze the cells present in the vitreous cavity. Based on this, they were classified as having ‘rare’ cells if there were less than 50 cells, ‘few’ cells if there were 60-194 cells, and ‘many’ cells if there were over 194 cells, which reflected a mean cell number of over 1 per B scan.
In patients whose eyes lacked a subhyaloid space, the ‘many’ cell category was defined as having more than 776 hyperreflective foci, which would correspond to over 4 cells per B scan, on average.
In contrast, when OCT scans from 14 individuals not known to have COVID-19 were assessed, 13 were found to have ‘rare,’ and one was found to have ‘few’ cells, respectively. The researchers consider that their findings indicate the presence of ongoing inflammation in nerve tissue even after a clinical recovery has occurred. This is intriguing since the vast majority of this group had mild COVID-19 without the need for hospitalization.
The presence of many cells in the vitreous is an abnormality, usually resulting from inflammation, hemorrhage, or a tumor. During the current study, 8 of those who reported complete recovery had ‘rare’ cells, while among those who still had symptoms, 2 had ‘few’ cells, and 2 had ‘many’ cells. Thus, incomplete subjective recovery was associated with more vitreous cells, indicating that inflammation persisted at other sites in the body.
Two participants had undergone SD-OCT scans at the same institution 6 months and 2 years prior to the current study. Both showed no or ‘rare’ cells at the time. It is noteworthy that both had hyperreflective foci on their post-COVID-19 scans.
This suggests, the researchers say, “that even ambulatory COVID-19 may lead to inflammatory cells persisting in the eye up to 1 month after recovery.”
Implications and Future Directions
The authors suggest that these findings may indicate the presence of post-viral inflammation complicating recovery from COVID-19, delaying symptomatic recovery for weeks from the first positive test, whether in young or in old patients.
The current study is limited by the use of SD-OCT imaging alone to identify inflammatory cells without molecular, cellular, or histologic confirmation. Secondly, the signs of inflammation in this condition may or may not be specific for COVID-19 alone, since this search for ocular inflammation on a subclinical scale has not been performed before, as far as is known, in patients convalescing from respiratory viral infections or other systemic diseases.
The study concludes, “A larger study is needed to determine the true prevalence of vitreous cells in persons recovering from COVID-19, and a longitudinal study is needed to determine its long-term ocular health sequelae.”

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.